- Author Rachel Wainwright [email protected].
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Viral warts
The content of the article:
- The reasons
- Types and symptoms
- Diagnostics
- Treating viral warts
- Home treatment
- Forecast
- Prevention
- Video
Viral warts are a viral infectious disease characterized by the appearance of small benign neoplasms (skin growths) on the skin and mucous membranes. It occurs quite often and affects people of any gender and age.

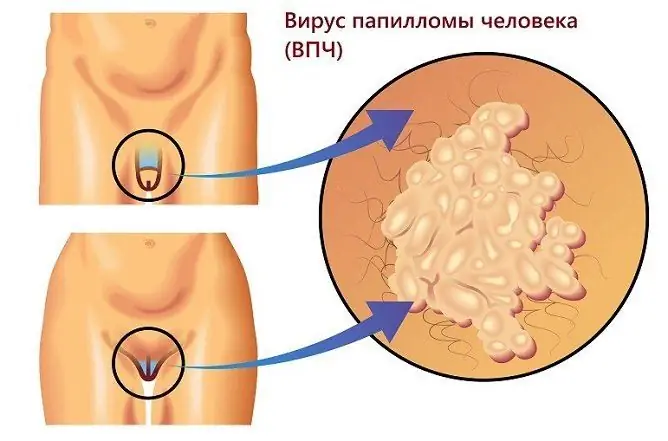
Viral warts are caused by the human papillomavirus (HPV)
The reasons
The causative agent of the disease is the human papillomavirus (HPV). Its various strains are capable of causing damage not only to the skin, but also to the mucous membranes of the vocal cords, bladder, oral cavity, external genital organs.
Infection occurs through contact with a sick or infected person, sick animals. The main routes of infection are:
- genital tract - typical for warts of the anogenital area (genital warts);
- vertical path - infection of a child from an infected mother during childbirth (it is the cause of genital warts and laryngeal papillomatosis in children);
- household way - the virus is able to maintain viability for a short time on objects used by a virus carrier or a sick person;
- autoinoculation (self-infection) - occurs during epilation, shaving.
The following factors increase the risk of infection:
- promiscuous sex life;
- frequent visits to saunas, swimming pools, gyms;
- work related to cutting raw fish or meat.
The human papillomavirus enters the body through minor injuries to the skin or mucous membranes. Then it enters the cells of the basal layer of the epithelium. Here it can be in one of two types:
- Episomal. HPV is located outside the chromosomal apparatus of the affected cell. This form of the disease is regarded as benign.
- Intrasomal. The virus is embedded (integrated) into the cellular genome. This form is considered malignant.
The incubation period is long: from 15 days to several years. Human papillomavirus infection is characterized by a latent, i.e., latent course. In the stage of clinical manifestations, that is, the actual formation of warts, it passes under the influence of various provoking factors (hypothermia, severe stress, poor living conditions), leading to a decrease in immunity.
In about 90% of patients with papillomavirus infection, self-healing occurs within a year from the moment of infection. In the rest, the disease takes on a recurrent long-term chronic course. In rare cases, warts may become malignant (infection with an oncogenic HPV strain).
Types and symptoms
Depending on the location and clinical signs, several types of viral warts are distinguished:
| View | Description |
| Vulgar (simple) | They account for approximately 70% of all types of viral warts. The disease often affects children and adolescents. Neoplasms are localized mainly on the fingers and the back of the hands. Much less often they are located on the face or mucous membranes. They have the appearance of dense rounded nodules, with a diameter of several mm to 1.5 cm. The color of the skin above them is not changed. |
| Plantar | Outwardly similar to the vulgar. They are located on the skin of the soles. They cause pain when walking. |
| Palmar-plantar |
Adults are amazed. Neoplasms look like small neoplasms that are dense to the touch. Wearing uncomfortable and tight shoes contributes to the spread of infection. This form of pathology requires a differential diagnosis with plantar syphilitic papules and common dry calluses. |
| Periungual | They are a variant of vulgar warts. Most often occurs in children biting burrs or biting nails. This form of the disease is characterized by the frequent occurrence of relapses. |
| Youth (flat) | They arise on the mucous membranes of the rectum and cervix, the skin of the hands and face, and the head of the penis. Most often occurs in adolescents and young people. |
| Filiform | They look like soft papules from flesh to dark brown in color. They appear on the skin of the eyelids, neck, mammary glands, axillary and groin areas. Education often has a leg, as a result of which the risk of injury increases. |
| Pointed (condylomas) |
Outwardly, they resemble cockscomb or cauliflower. Surface color from flesh to pink. When rubbed, they turn crimson red. Bleed easily when injured. They are localized in the anogenital region, and in children they can also be located in the area of the nasolabial folds. Warts are characterized by the presence of a thin stem, as well as a tendency to form large conglomerates. |
Diagnostics
Diagnostics is carried out according to the characteristic appearance of the formations. Differential diagnosis with the following diseases is required:
- lichen planus;
- warty form of skin tuberculosis.
In carrying out differential diagnostics, special atlases are of great help, in which photos of various types of skin diseases are presented. In difficult diagnostic cases, a biopsy is performed, followed by a histological analysis of a tissue sample.
Treating viral warts
One of the following methods is used to remove viral warts:
- Removal by laser. After performing local anesthesia using a laser beam, layer-by-layer burning of the neoplasm is performed. The wound heals within 10-15 days without scarring.
- Electrocoagulation. It is performed under local anesthesia. With a metal electrode in the form of a loop, the wart is cut off near the very base and the tissue is cauterized (coagulated). A dense dark crust forms on the wound, which disappears after 7-10 days. If the lesion is large, a barely noticeable scar may remain on the skin.
- Cryodestruction. The method is based on the destruction of pathological tissue by freezing it with liquid nitrogen.
If a large area of skin is affected, it may need to be excised. The operation is performed under local anesthesia. The wound is closed with cosmetic subcutaneous sutures, as a result of which a very thin and almost invisible scar forms in its place.
In the postoperative period, in order to possibly prevent the spread of infection, it is recommended to lubricate the intact skin around the wound with antiviral ointment (selected by the doctor).
For the prevention of recurrence of the disease, antiviral and immunomodulatory therapy is usually prescribed.

It is better to remove warts in a medical institution using one of the minimally invasive methods.
Home treatment
You should not try to get rid of warts at home using traditional therapies. They are not only ineffective in most cases, but can also lead to the development of a number of complications:
- wound infection with the development of purulent inflammation;
- spread to healthy areas of the skin;
- bleeding.
In some cases, viral warts can develop into malignant tumors. Therefore, when they are removed, a histological examination is required, which is not possible to perform at home.
Thus, you should not try to get rid of viral warts on your own. It is necessary to consult a doctor and carefully follow all his prescriptions and recommendations.
Forecast
According to various authors, the effectiveness of treatment of viral warts is 50-94%. The likelihood of recurrence of the disease in the long term is 25%.
Prevention
Prevention of human papillomavirus infection is based on careful adherence to the rules of personal hygiene (especially carefully when visiting swimming pools, gyms, baths and saunas) and avoiding promiscuous sexual intercourse.
Video
We offer for viewing a video on the topic of the article.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
Found a mistake in the text? Select it and press Ctrl + Enter.