- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Leukoplakia of the cervix
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease symptoms
- Diagnostics
- Treatment of cervical leukoplakia
- Potential consequences and complications
- Forecast
- Prevention
Leukoplakia of the cervix is a pathological change in a limited area of the outer part of the cervix (exocervix), manifested by keratinization and proliferation of cells of the stratified epithelium of varying severity (acanthosis, parakeratosis, hyperkeratosis). When examining the cervix in the mirrors, leukoplakia foci look like whitish plaques towering above the unchanged surface of the exocervix. In some patients, similar plaques are located on the mucous membrane of the cervical canal.

Foci of leukoplakia of the cervix can be multiple or single.
Leukoplakia of the cervix is a widespread pathology that most often affects women of reproductive age. In the general structure of all diseases of the cervix, the share of leukoplakia accounts for 5.5%.
Leukoplakia of the cervix is considered a precancerous disease. This is due to the fact that in about 32% of patients, malignancy of epithelial cells occurs in the lesions. Issues related to early diagnosis and treatment of cervical leukoplakia are an urgent problem of modern gynecology and oncology, as they are directly related to a decrease in the incidence of cervical cancer.
Causes and risk factors
Both exogenous factors (traumatic, chemical, infectious) and endogenous (disorders of the immune and hormonal regulation of the body), as well as their combination, can lead to the development of cervical leukoplakia.
In the formation of violations of the hormonal background of a woman's body, great importance belongs to the failure of the correct relationship between the hypothalamus, pituitary gland, ovaries and uterus, which is accompanied by a deficiency of progesterone, absolute or relative hyperestrogenism, anovulation. The outcome of such hormonal disorders is the launch of hyperplastic processes in the target organs.
The contributing factors are:
- infectious and inflammatory diseases of the genital organs (adnexitis, endometritis, cervicitis, colpitis);
- disorders of menstrual function (oligomenorrhea, amenorrhea);
- promiscuous sex life;
- sexually transmitted infections (chlamydia, trichomoniasis, herpes, papillomavirus infection, mycoplasmosis, ureaplasmosis, cytomegalovirus infection);
- decrease in general and local immunity;
- chemical and traumatic damage to the cervix that occurs during medical procedures (diagnostic curettage, artificial termination of pregnancy, diathermocoagulation or drug cauterization of cervical erosion).
Normally, the cells of the stratified epithelium of the outer part of the cervix do not keratinize. However, under the influence of provoking factors, a keratisation mechanism is triggered in them, as a result of which a gradual restructuring (disintegration of intracellular organelles and nuclei) begins in the epithelial cells, leading to the formation of horny scales, which lack glycogen.
Forms of the disease
Based on the features of the morphological structure, leukoplakia of the cervix is divided into two types:
- simple - refers to background changes (para- or hyperkeratosis). In the lesion focus, thickening and keratinization of the surface layers of the multicellular epithelium occurs, while the epithelial cells of the basal and parabasal layers remain unchanged;
- proliferative - characterized by impaired proliferation and differentiation of cells of all layers, the appearance of atypical structural elements. It is a precancerous process called cervical intraepithelial neoplasia (cervical dysplasia, CIN).
Disease symptoms
Leukoplakia of the cervix is asymptomatic and is not accompanied by any complaints from the patient, therefore it is detected only during a routine gynecological examination. In very rare cases, against the background of cervical leukoplakia, patients develop leucorrhoea with an unpleasant odor or slight bleeding after intercourse.
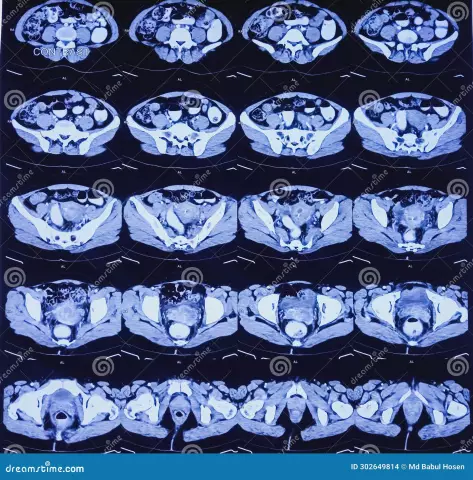
Diagnostics
Diagnosis of cervical leukoplakia is not difficult and is carried out during a gynecological examination. When examining the neck in the mirrors, whitish plaques or spots of different sizes, oval shapes and with clear boundaries are found on it. They may rise slightly above the surface of the unchanged mucous membrane of the cervix. Sometimes the surface of the plaques is covered with small scales (keratinized epithelial cells).
The prevalence and size of leukoplakia foci varies from a single point plaque to extensive multiple zones that completely cover the outer part of the cervix, pass to the mucous membrane of the cervical canal and vaginal vaults.
In order to confirm the diagnosis, a cytological examination of scraping from the surface of the plaque is performed. Detection of accumulations of epithelial cells with signs of parakeratosis or hyperkeratosis is characteristic.

When performing scraping against the background of para- and hyperkeratosis, it is not possible to capture the cells of the deep layers of the mucous membrane of the exocervix, in which differentiation disorders, atypia can be noted. In this regard, a knife targeted biopsy is performed, followed by a histological analysis of the resulting tissue. This method allows you to either exclude or confirm the presence of cervical intraepithelial neoplasia, a tumor process.
Given that leukoplakia is a precancerous disease, all patients are shown curettage of the cervical canal in order to exclude a malignant tumor of the cervix.
To clarify the nature and size of the epithelial lesion, an extended colposcopy (video colposcopy) is performed. At the same time, white plaques are observed with smooth, clear edges, a fine-grained surface and the absence of blood vessels.
When lubricated with Lugol's solution, the surface of the plaques does not stain (Schiller's test).
In order to identify the reasons that led to the development of cervical leukoplakia, patients are prescribed according to indications:
- research of hormonal and immune status;
- bacteriological examination of discharge from the cervix;
- microscopic examination of the detachable cervical canal;
- serological studies aimed at identifying sexually transmitted infections.
Leukoplakia of the cervix requires differential diagnosis with cervical erosion, cervical cancer. If necessary, patients are referred for a consultation with an endocrinologist or oncologist.
Treatment of cervical leukoplakia
The choice of treatment for cervical leukoplakia depends on the form of the disease (simple or proliferative). The purpose of the therapy is the complete removal of pathological foci and the elimination of diseases that caused their occurrence.
If indicated, women are prescribed anti-inflammatory, antiviral or antibacterial therapy. The following methods are used to remove foci of leukoplakia of the cervix:
- chemical coagulation;
- diathermocoagulation;
- CO 2 -laser vaporization;
- argon plasma coagulation;
- radio wave destruction;
- cryogenic impact.
The procedure for the destruction of leukoplakia foci of the cervix is performed on an outpatient basis, under local anesthesia. The duration of tissue healing depends on the method of destruction used, concomitant diseases, lesion area and ranges from 14 to 60 days.
Until complete epithelialization of the cervix, sexual activity and the use of any methods of contraception are prohibited.
Indications for surgical intervention (amputation of the cervix, conization of the cervix) is a combination of leukoplakia with kraurosis, hypertrophy, cicatricial deformities of the cervix, or the diagnosis of cervical intraepithelial neoplasia in the patient.
Potential consequences and complications
The main complication of cervical leukoplakia is malignancy of the lesion with the development of cervical cancer.
Forecast
With timely treatment of cervical leukoplakia and provided that the patient does not have papillomavirus infection, atypia, and the elimination of adverse factors, the prognosis is favorable.
In cases where the root causes of the disease remain unresolved, relapses and the transformation of foci into a cancerous tumor are not excluded.
With simple leukoplakia of the cervix, patients of childbearing age are treated with sparing methods (chemical coagulation, radiosurgical treatment, laser vaporization, cryodestruction), which prevents deep tissue damage. If in the future the patient becomes pregnant, systematic medical monitoring of the state of the cervix is necessary.
Prevention
Prevention of cervical leukoplakia includes the following measures:
- timely treatment of infectious and inflammatory diseases of the reproductive system;
- prevention of abortion;
- rational management of childbirth and accurate performance of medical gynecological manipulations, which reduces the risk of damage to the cervix;
- prevention of infection with sexually transmitted infections (use of barrier methods of contraception, refusal of casual sex).
Patients with menstrual irregularities should be registered with a gynecologist-endocrinologist and receive appropriate treatment aimed at correcting hormonal levels.
Prevention of cervical leukoplakia also includes health education among women, explaining the importance of regular gynecological examinations. Vaccination is also recommended for patients to prevent infection with the human papillomavirus (HPV).

After completing the course of treatment for cervical leukoplakia without atypia, the patient should be registered with a gynecologist. Every six months, an HPV test, a smear examination for oncocytology, and colposcopy are performed. In the absence of relapses of the disease, after two years, the patient is removed from the dispensary registration and transferred to the usual observation regime.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!