- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Tooth cyst
The content of the article:
- Characteristics of the neoplasm
- Why arises
-
Treatment of a cyst on a tooth
- Surgery
- Conservative therapy
- Possible consequences
- Video
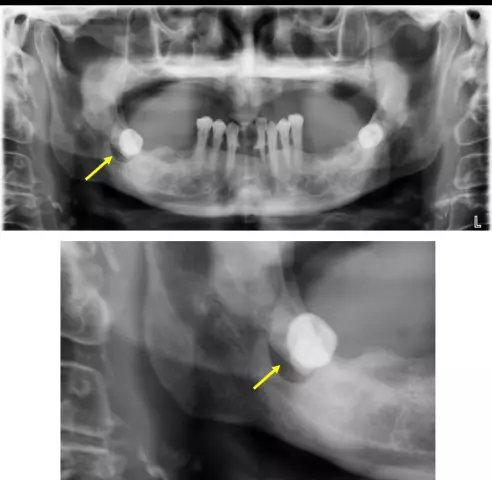
A tooth cyst is an inflammatory formation, often filled with serous fluid and having a direct affinity for dental tissues. It can occur in the root area, apex or in the area of the lateral tooth surfaces. Refers to benign neoplasms (not to be confused with tumor-like processes in the jaw such as granulomas).

A root cyst of a tooth develops as a result of the spread of infection to the tissues surrounding the root
Characteristics of the neoplasm
- The cavity is surrounded by a dense fibrous capsule.
- The content can be serous, purulent, hemorrhagic.
- Sizes vary widely (it can cover several teeth).
- Localization for each option is individual.
- At an external examination or in a photo, the gum tissue may be intact, since external manifestations of the type of hyperemia, edema appear only with suppuration.
- In 85% of cases, the process is caused by an infection in the dental tissue (caries).
- Severe clinical picture (pain of varying intensity, symptoms of intoxication, headaches).
- There is no pronounced dependence on age or gender.
Why arises
There are the following causes of a tooth cyst (in each individual variant of occurrence, one of the reasons dominates):
- Inflammatory diseases of dental tissues (pulpitis, periodontitis). In this case, the inflammation captures the adjacent tissues, a cavity is formed in them, in which the inflammatory exudate accumulates.
- Inflammatory diseases of adjacent organs (sinusitis, sinusitis, otitis media). In this case, the inflammatory agent enters the dental tissues by contact or hematogenous route.
- Poor quality dental care (preservation of carious foci with subsequent filling). It is also possible the appearance of cystic formations during tooth extirpation (incomplete removal, preservation of the cyst membranes).
- Disruption of the immune system. Conditionally pathogenic flora of the oral cavity with minor injuries can become a source of inflammation.
- Traumatic injury. In this case, the cystic cavity is more likely to be classified as post-traumatic than true. Such formations are more often hemorrhagic, are not associated with dental tissues and rarely suppurate.
- Disruption of the teething process. In adults, this phenomenon often occurs when wisdom teeth appear. It is more often localized in the retromolar region and is associated with the formation of a bone pocket, which is filled with fibrous and epithelial tissue. With inflammation, the cells of these tissues begin to divide, and a cystic cavity gradually forms.
- Violation of the developmental processes of the tooth germ. In this case, chronic periodontitis of deciduous teeth occurs. Around the crown of an unerupted tooth, a focus of intensively dividing epithelial cells is formed (at any stage of tooth formation, which leads to a violation of its structure). This explains the presence of rudimentary tissue (tooth-containing cysts) in such a cystic cavity.
A dentist (in some cases, a maxillofacial surgeon) conducts diagnostics (X-rays in various projections), and, depending on the specific factor that led to the formation of the cystic cavity, sets the treatment regimen.
Treatment of a cyst on a tooth
The treatment uses:
- surgical method (removal);
- conservative method (more often serves as an addition to the operation).
Surgery
In surgical practice, it is customary to divide cystic neoplasms into two types:
- odontogenic, which are inflammatory in nature (root, tooth-containing, paradental);
- odontogenic, which are malformations (follicular, eruption).
The following options for removing a cyst on a tooth are carried out, depending on the type:
| Operation | Technics |
| Cystectomy (in this way, neoplasms are removed that belong to developmental defects) |
The method involves the removal of all cystic formation with membranes. Pain relief: local anesthesia in combination with neuroleptanalgesia. The operation is done as follows: 1. Using a scalpel, cut out the muco-periosteal flap. The shape may vary depending on the characteristics of the cyst (trapezium most often). The edges of the incision overlap the boundaries of the bony edges by 0.5-1 cm. 2. Using a special tool, the flap is removed from the jaw bones. 3. Trepanation is performed until the cyst wall is isolated. 4. The cyst is excised together with the membranes, and the sections of the roots of the teeth, which are projected into the cyst cavity, are also resected. The tops of the roots are removed up to the bony walls of the cavity (sometimes the teeth must be completely removed). 5. The bone cavity is washed with antiseptics. 6. Provides a thorough hemostasis. 7. The flap is placed in place and fixed with interrupted sutures (sometimes drainage is left). The removed cystic walls and contents are sent for cytological examination. |
| Cystotomy (this method is used mainly in relation to cystic neoplasms of an inflammatory nature) |
The essence of the surgical intervention consists in excision of the anterior cystic wall, so that adequate drainage of the formation is achieved. The method is more often used in children in order to preserve the rudiments of permanent teeth. Execution stages: 1. The same mucoperiosteal flap is cut out as in the previous treatment option, but in this case the incision edges do not overlap the boundaries of the bony edges. 2. Similarly, all soft tissues are removed until the cystic bone is exposed. 3. Only the anterior wall of the formation should be removed. 4. A tooth that will cause inflammation must be removed or partially resected. 5. The cavity is washed with antiseptics, hemostasis is provided. 6. At the last stage, the flap is placed in the bone cavity and fixed. A turunda soaked in an aseptic solution is also placed in the cavity. As the healing progresses, the cavity will fill with connective tissue and decrease (washing and changing the turunda are carried out 2 times a week until complete healing). |
| Oronasal cystectomy (in case of sinus involvement) |
The essence of the operation is to connect the sinus of the upper jaw, cysts and lower nasal passage. Operation stages: 1. Dissection with a scalpel of the mucosa and periosteum to the bone. The incision does not reach the transitional fold by 0.5 cm and is made in the area located in the region of the second incisor and up to the third large molar. 2. The anterior part of the sinus is opened and the membranes of the cyst are removed with partial resection of the roots of the teeth. 3. Only the affected areas of the mucous membrane are removed, an anastomosis is created with the lower nasal passage. 4. The wound is sutured in layers on the eve of the oral cavity. Gradually, the cystic cavity begins to fill with connective tissue and heal. |
| Oronasal cystotomy (if sinus involvement) | It is not a radical treatment. Used in children. In this case, only the upper and anterior walls of the cyst lie down, the roots of the teeth are not removed or resected. |
|
Plastic cystectomy (used for defects, pronounced bone changes in bone tissue) |
The most non-dramatic type of intervention. Refers to organ-preserving operations. They are used more often with pronounced suppurative processes. It is a combined form of surgery, in which a complete excision of the cyst is performed, but the wound is not sutured, but tamponed. It is carried out in two stages: I. All stages of classical cystotomy (creation of communication with the oral cavity and drainage, that is, removal of signs of inflammation). II. All stages of cystectomy are performed 1-1.5 years after the first stage. |
There are several features of the treatment of festering cystic formations:
- no incisions are made in the area of the future mucoperiosteal flap;
- a puncture is made along the alveolar ridge for adequate outflow and drainage;
- elective surgery is indicated after the inflammation subsides.
The following complications of surgical treatment are possible:
- bleeding or suppuration of a postoperative wound;
- traumatic damage to the nerve plexuses;
- perforation of the sinuses;
- divergence of the edges of the wound due to repeated suppuration;
- postoperative paresthesias;
- necrotic changes in the surrounding tissues.

Surgical removal is the most effective treatment for a dental cyst
Conservative therapy
Non-surgical treatments include:
- The introduction of antibiotics directly into the root canal (an option for removing root cystic formations, which has a high recurrence rate).
- Depophoresis is another option, in which a special gel-like substance is injected into the dental cavity, after which electrophoresis is resorted to. Provides antibacterial effect.
- Laser exposure. The essence of the method is related to the introduction of special laser equipment into the dental canal and "sealing" of the cystic cavity wall with simultaneous disinfection of the affected area.
Possible consequences
With late treatment or its absence, dental cystic neoplasms can have a number of complications:
- Purulent fusion of bone tissue (especially for cysts at the root of the tooth). The result can be the development of osteomyelitis of the lower jaw due to the ingress of pus deep into the bone. In rare cases, pathological fractures or cracks are possible due to thinning of bone tissue.
- The transition of inflammation to an abscess or phlegmon. In this case, the purulent focus is significantly widespread.
- Regional lymphadenitis, or inflammation of regional lymph nodes. As a rule, it passes without a trace when the cause is eliminated.
- Sinusitis or sinusitis with localization of the cyst in close proximity to the walls of the sinuses.
- Sepsis. A very dangerous complication that appears only against the background of an extensive purulent lesion does not cause it by itself.
A cyst rarely gives serious consequences after a course of treatment.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!