- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Myopathy
The content of the article:
- Causes and risk factors
- Forms of the disease
- Myopathy symptoms
-
Diagnostics
Differential diagnosis
-
Treatment of myopathies
- Drug therapy
- Physiotherapy
- Orthopedic treatment
- Surgery
- Psychological support
- New in the treatment of myopathies
- Treatment of acquired myopathies
- Possible complications and consequences
- Forecast
- Prevention
- Video
Myopathy is a disease of predominantly hereditary origin, which is based on degenerative muscle damage with their progressive atrophy.
This is a rare disease that nevertheless occurs everywhere, affecting people regardless of region of residence and race. According to available data, every 3500th boy is born with pseudohypertrophic myopathy, or Duchenne myopathy.
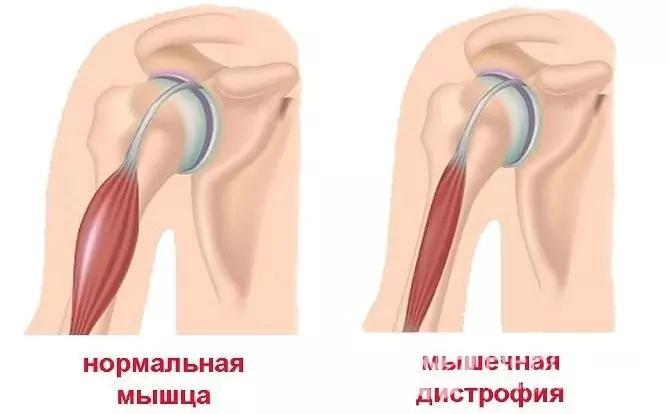
Myopathy is characterized by muscular dystrophy and then atrophy
Causes and risk factors
Primary myopathy is a genetically determined disease. The direct mechanism that triggers a chain of pathological reactions and leads to metabolic disorders in muscle cells is still unclear. According to the existing theory of defective membranes, the primary pathology lies in the plasma membrane of muscle fibers, which leads to the uncontrolled penetration of calcium, which activates enzymes (proteases) that destroy muscle tissue. There is an increase in the level of creatine phosphokinase, which leads to the inability of the muscles to retain and bind creatine; decreases the content of ATP (adenosine triphosphate, the main donor of cellular energy), resulting in atrophy of muscle fibers.
Often, manifestations of myopathy arise (as well as those that already exist) under the influence of unfavorable provoking factors, which include:
- infectious diseases;
- intoxication;
- physical and psycho-emotional overstrain.

Most myopathies are hereditary, some of them are associated with the X chromosome
Acquired forms of myopathy are caused by diseases that cause nerve damage, metabolic disorders, toxic effects, intense inflammatory or tumor processes.
Forms of the disease
There are several classifications of the disease, but none is considered complete.
Distinguish between primary and acquired myopathies. In most cases, when it comes to this disease, hereditary, or primary myopathy is meant.
Acquired myopathy, depending on the origin, is:
- thyroid - can accompany both hyper- and hypothyroidism;
- steroidal - caused by inadequate intake of steroid-containing drugs (especially fluoride corticosteroids) for another disease;
- alcoholic - a history of alcoholism is determined, the disease is often accompanied by cardiomyopathy, unlike other forms, pain may be present;
- polymyositis (in turn, it can be idiopathic or secondary).
Hereditary myopathies are divided into:
- muscular dystrophies - they are characterized by primary damage to muscle fibers;
- amyotrophies (spinal and neural) - caused by a violation of muscle innervation due to damage to the central (spinal motor neurons) or peripheral nervous system.
From the clinical and genetic point of view, hereditary myopathies are usually divided into three large groups:
- pseudohypertrophic, or Duchenne myopathy.
- shoulder-scapular-facial, or Landusi myopathy - Dejerine.
- juvenile, or Erb's myopathy.
Later, new ones were added to these classic forms:
- scapular-peroneal amyotrophy of Davidenkov;
- distal late hereditary Welander myopathy;
- ophthalmic;
- benign X-chromosomal, or Becker's myopathy;
- congenital (congenital) non-progressive;
- McArdle disease; and other, more rare forms.
Myopathy symptoms
| Disease form | Genetic conditioning | Characteristic signs |
| Duchenne myopathy | The recessive type of inheritance linked to the X chromosome, only boys get sick, the disease is transmitted from an apparently healthy mother. |
Myopathy in a child makes its debut early (the first 5 years of life), at first the muscles of the pelvis and lower extremities are involved in the atrophic process with the development of severe pseudohypertrophy of the calf muscles. In about a third of patients, there is a decrease in intelligence (slight debility), which does not tend to progress. A high level of aldolase, transaminase and creatine kinase is determined in blood serum. Mothers carrying the abnormal gene also have elevated serum enzyme levels. The disease progresses rapidly and inevitably, leading to death from dystrophy or respiratory infections. Patients rarely live longer than 20 years. |
| Shoulder-scapular-facial | Autosomal dominant inheritance. | It can make its debut at any age, but more often begins in adolescence. Characterized by proximal atrophy on the upper limbs and distal - on the lower. One of the specific symptoms is pterygoid scapula. Severe lordosis of the lumbar spine may develop. Slight or moderate sensory impairment in the distal extremities is observed. |
| Juvenile | Autosomal recessive inheritance. | The most common type of hereditary myopathy. Atrophy begins with the muscles of the pelvic girdle and lower extremities, has a tendency to generalization and early leads to immobility of patients. |
| Late distal | Dominant type of inheritance. | Debuts after 20 years. Atrophy begins in the small muscles of the hands and feet, then affects the muscles of the forearms and legs. It progresses slowly. |
| Ophthalmic | Inheritance can be either autosomal dominant or autosomal recessive, in the latter case, the disease is more severe. | Some cases fall under the definition of chronic progressive ophthalmoplegia, in others, atrophy of the muscles of the soft palate, larynx, tongue, masticatory and facial muscles joins the initial bilateral ptosis of the eyelids and eyes. |
| Becker's myopathy | The type of inheritance is recessive, linked to the X chromosome. The sons of people suffering from this form of myopathy are free of the pathological gene, and the daughters are heterozygous carriers. | It resembles the ophthalmic form, but begins later, progresses more slowly, has a benign course. |
| Congenital (congenital) | The type of inheritance is mostly recessive. | They are characterized by congenital muscular hypotonia. The course is benign. This is a group of myopathies that require further study. |
| Congenital structural | Different types of inheritance. | Debut at any age, however, in the overwhelming majority of cases - early (at birth or in the first months of life), generalized muscle hypotonia, muscle atrophy, absence or decrease in tendon reflexes, structural skeletal abnormalities. |

Duchenne myopathy is characterized by pseudohypertrophy of the calf muscles, this form is also called pseudohypertrophic
The following symptoms are common to most myopathies:
- Muscle weakness appears and slowly builds up, having a bilateral (symmetrical) character.
- There are no paresthesias (disturbances of sensitivity in the form of tingling, burning, creeping) in the limbs.
- No muscle soreness despite increasing weakness.
- To a greater extent, weakness affects the proximal (upper) parts of the extremities (distal, or lower ones are more often affected by polyneuropathy of various etiologies). This is manifested by the fact that it becomes difficult to climb stairs, comb, wash.
- Absence of dysfunction of the pelvic organs.
- Absence of violations of deep reflexes (occasionally they can be slightly reduced).
- Weakness of the facial muscles manifests itself in the inability to stretch the lips for a whistle or kiss, the inability to close (or, on the contrary, open wide) eyes.
Diagnostics
Antenatal detection of pathology is possible according to the results of a study of amniotic fluid (amniocentesis).
Diagnosis of familial forms and typical cases of myopathy is usually straightforward. Clinical examination reveals muscle weakness, which usually changes throughout the day. The patient is asked to puff out their cheeks, stretch their lips, close their eyes, and then quickly open their eyes (causing difficulty). Check for double vision, dysarthria, dysphagia. The strength of the iliopsoas and deltoid muscles, flexor and extensor muscles of the neck (flexors are weaker than extensors) is examined.
In doubtful cases, resort to the following diagnostic methods:
- needle electromyography - a myopathic pattern is determined, which is characterized by a reduced amplitude of the M-response, with increased interference and polyphasic potential;
- magnetic resonance imaging (MRI) of muscles - fatty and / or connective tissue degeneration of muscle fibers is determined;
- muscle biopsy - allows you to confirm the diagnosis and differentiate a number of myopathies;
- study of creatine-creatinine metabolism - myopathy is characterized by the presence of creatinuria, an increase in the level of creatine kinase in the blood serum (especially with pseudohypertrophic myopathy);
- genetic research, including molecular genetic analysis, genetic testing of family members, especially those capable of childbearing.

Electromyography - a method used in the diagnosis of myopathies
In acquired myopathies, the diagnostic search depends on the root cause, for example, in the thyroid form, the level of thyroid hormones is determined.
Differential diagnosis
Congenital myopathies in children should be differentiated from the atonic-astatic form of infantile cerebral palsy (cerebral palsy) and dysplastic kyphoscoliosis of unknown etiology.
Treatment of myopathies
Currently, there is no cure for congenital myopathy, but adequate therapy helps to cope with the symptoms of the disease and slow its progression. Patients with myopathy should be monitored by a physician, neurologist, cardiologist, and orthopedist. Treatment is long-term, in most cases life-long. Patients receive it both on an outpatient basis and in a hospital. Control is periodically carried out by conducting an examination, and, if necessary, changes are made to the therapy regimen.
Drug therapy
Treatment of hereditary myopathies aims at:
- Correction of metabolic processes and microcirculation in muscles and nervous system.
- Normalization of the functions of the nervous system.
For this purpose, anabolic steroids, trophotropic drugs, biogenic stimulants, vitamins, potassium preparations, anticholinesterase and vasoactive agents can be prescribed.
The duration of each comprehensive course is 4-6 weeks; it may include, for example, the following drugs:
- Alpha-tocopherol in the form of intramuscular injections of 0.3-1 ml for 30 days;
- ATP (adenosine triphosphoric acid) intramuscularly 1 ml for 30 days;
- Glutamic acid - 0.5-1 g 3 times a day for a long time;
- Nivalin 0.25% solution 0.1-2 ml, depending on age;
- Proserin 0.05% solution subcutaneously 1 ml for 30 days;
- Dibazol 1% 1 ml;
- Oksazil;
- B vitamins (B6, B12);
- ACTH 5-10 U 4 times a day for two weeks with muscle retraction.
A good therapeutic effect is demonstrated by blood transfusions, 100-150 ml of blood is transfused once a week for 4-6 weeks.
Physiotherapy
The following methods are used:
- iontophoresis with calcium;
- electrophoresis;
- X-ray therapy of the diencephalic area;
- ultrasound effect on muscles;
- electrical muscle stimulation;
- massage;
- passive stretching of the tendons.
Physiotherapy exercises (exercise therapy) are used. Regular exercise can slow the progression of the weakness and contracture that occurs in advanced myopathy, but care must be taken to avoid overstraining the weakened muscles. An effective option for adequate physical activity is swimming in the pool under the supervision of an exercise therapy instructor (physiotherapist).
Orthopedic treatment
In some cases, orthopedic correction of spinal deformities is indicated with the help of special lightweight corsets or orthopedic shoes.
Surgery
In some cases, surgical treatment is advisable, which consists in lengthening the shortened tendons.
Psychological support
One of the important elements of treatment is psychological support for patients, both family and professional. Their loved ones should also receive psychological help.
New in the treatment of myopathies
The search for new methods and effective means of treating both hereditary and acquired forms of the disease is constantly being carried out. Current trends are cell and gene therapy. Myopathies associated with metabolic disorders are quite successfully treated with the help of means that compensate for the lack of one or another enzyme. Thus, the new drug Translarna has demonstrated high efficiency in the treatment of Duchenne's disease.
Translarna is a drug used in the treatment of Duchenne myopathy
Treatment of acquired myopathies
The treatment of acquired myopathies, or myopathic syndromes, is generally the same, but the main task is to eliminate the underlying pathology. For example, an important condition for the treatment of alcoholic myopathy is a complete rejection of alcohol and detoxification, thyroid - correction of thyroid hormones, steroid - refusal of causal drugs.
Possible complications and consequences
The consequences of myopathy are associated with dysfunction of different muscle groups, for example, cardiomyopathy leads to heart failure, myopathy affecting the intercostal muscles - to a deterioration in lung function with all the ensuing consequences. Neurological disorders develop. Gradually, the body weakens, the functions of the immune system decrease, due to which patients suffer from frequent infectious diseases, which in some cases are the direct cause of death.
Forecast
The prognosis depends on the form of the disease. It is unfavorable for pseudohypertrophic myopathy, which quickly leads to severe disability and early death. The prognosis for myopathies that debut later, at the end of adolescence, is more favorable.
Prevention
It is not possible to prevent the appearance of congenital myopathy. Identifying the defective gene can help plan pregnancy for people with a family history of inherited disease.
Preventive measures are effective for acquired myopathies. They consist in refusal of self-medication, refusal of alcohol abuse, timely detection and treatment of thyroid diseases, prevention of intoxication.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!

