- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Hepatitis B
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
- Symptoms
- Diagnostics
-
Treatment
- Acute hepatitis B
- Chronic hepatitis B
- Possible complications and consequences
- Forecast
- Prevention
Hepatitis B (serum hepatitis) is a viral liver disease in which the death of hepatocytes occurs due to autoimmune mechanisms. As a result, the detoxification and synthetic functions of the liver are impaired.
According to WHO estimates, over 2 billion people in the world are infected with the hepatitis B virus; 75% of the world's population lives in regions with a high incidence rate. Acute infection is diagnosed in 4 million people every year. In recent years, there has been a decrease in the incidence of hepatitis B, which is due to the vaccination.
Hepatitis B virus is highly virulent
Causes and risk factors
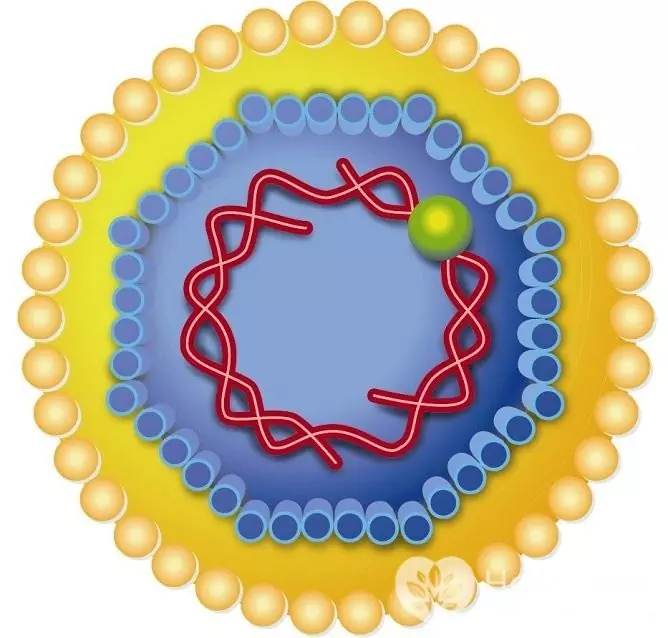
The hepatitis B virus belongs to the hepadnavirus family. It is very resistant to physical and chemical attack and has a high degree of virulence. After suffering a disease, a person develops a persistent lifelong immunity.
In patients and virus carriers, the pathogen is contained in biological fluids (blood, urine, semen, saliva, vaginal secretions), is transmitted from person to person by parenteral route, that is, bypassing the gastrointestinal tract.
The hepatitis B virus is highly resistant to chemical and physical attack
Previously, infection often occurred as a result of medical and diagnostic manipulations, transfusion of blood and blood products, manicure, and tattooing. In recent decades, the sexual transmission of infection has become predominant, which is explained by the following factors:
- widespread use of disposable instruments for invasive procedures;
- application of modern methods of sterilization and disinfection;
- thorough examination of blood donors, sperm;
- sexual revolution;
- the prevalence of injecting drugs.
With unprotected sexual contact with a sick person or a virus carrier, the risk of contracting hepatitis B, according to various sources, ranges from 15 to 45%. Injecting drug users play an important role in the spread of the disease - about 80% of drug addicts are infected with the hepatitis B virus.

About 80% of injecting drug users are infected with hepatitis B virus
There is a common way of infection: transmission of the virus occurs as a result of the use of common toothbrushes, manicure tools, blades and razors, bath accessories and towels. Any (even minor) injuries to the skin and mucous membranes in this case become the entrance gate of the infection. If the rules of personal hygiene are not followed for several years, all family members of the virus carrier become infected.
The vertical route of transmission of infection, that is, infection of the child from the mother, is more often observed in regions with a high incidence. With a normal pregnancy, the virus does not cross the placental barrier, and infection of the baby can occur during childbirth. However, with some pathologies of the development of the placenta, its premature detachment, intrauterine infection of the fetus is not excluded. If HBe antigen is detected in a pregnant woman's blood, the risk of infection of a newborn is estimated at 90%. If only HBs antigen is detected, the risk of infection is less than 20%.
Viral hepatitis B is also transmitted through transfusion of infected blood or blood components to the recipient. All donors undergo mandatory diagnostics, but there is a serological window, that is, a period when a person is already infected and poses an epidemiological danger to others, but laboratory tests do not reveal infection. This is due to the fact that from the moment of infection to the moment of production of antibodies, which are markers of the disease, it takes from 3 to 6 months.
The risk group for hepatitis B includes:
- injecting drug users;
- persons receiving blood transfusion;
- persons with promiscuous sex life;
- medical workers who, in the course of their professional activities, are in contact with the blood of patients (surgeons, nurses, laboratory assistants, gynecologists).
Airborne transmission of the hepatitis B virus is not possible.
Forms of the disease
According to the duration of the course of the disease, an acute and chronic form is distinguished. According to the peculiarities of the clinical picture, hepatitis B is:
- asymptomatic;
- anicteric;
- jaundiced.
Disease stages
There are the following stages of hepatitis B:
- Incubation period. Duration - from 2 to 6 months, more often - 12-15 weeks, during which active replication of the virus occurs in the liver cells. After the number of viral particles reaches a critical value, the first symptoms appear - the disease progresses to the next stage.
- Prodromal period. The emergence of nonspecific signs of an infectious disease (weakness, lethargy, pain in mice and joints, lack of appetite).
- It's high. The appearance of specific signs (the liver increases in size, icteric staining of the sclera and skin appears, intoxication syndrome develops).
- Recovery (convalescence) or the transition of the disease into a chronic form.
Symptoms
The clinical picture of hepatitis B is caused by impaired outflow of bile (cholestasis) and impaired liver detoxification function. In some patients, the disease is accompanied by endogenous intoxication, that is, poisoning of the body with products of disturbed metabolism caused by necrosis of hepatocytes. In other patients, exogenous intoxication prevails, resulting from the absorption into the bloodstream of toxins formed in the intestines during digestion.
With any type of intoxication, the central nervous system is the first to suffer. Clinically, this is manifested by the appearance of the following cerebrotoxic symptoms:
- sleep disturbance;
- increased fatigue, weakness;
- apathy;
- disturbances of consciousness.
In severe forms of the disease, hemorrhagic syndrome may develop - recurrent nosebleeds, increased bleeding of the gums.

The clinical picture of hepatitis B
Violation of the normal outflow of bile causes jaundice. When it appears, the general condition worsens: the manifestations of asthenia, dyspepsia, hemorrhagic syndrome increase, and excruciating itching occurs. The feces become lighter, and the urine, on the contrary, darkens and resembles dark beer in color.
Against the background of an increase in jaundice, an increase in the liver (hepatomegaly) occurs. In about 50% of cases, in addition to the liver, the spleen is enlarged. Normal liver sizes with severe jaundice are considered an unfavorable prognostic sign.
The icteric period lasts for a rather long time, up to several months. Gradually, the condition of the patients improves: the phenomena of dyspepsia disappear, the icteric symptoms regress, the liver returns to normal size.
In about 5-10% of cases, viral hepatitis B becomes chronic. Its signs:
- mild intoxication;
- subfebrile temperature;
- persistent enlargement of the liver;
- a persistent increase in the activity of hepatic transaminases and an increased level of bilirubin.
Diagnostics
Diagnosis of viral hepatitis B is based on the detection of specific antigens of the virus (HbeAg, HbsAg) in the blood serum, as well as the detection of antibodies to them (anti-Hbs, anti-Hbe, anti-Hbc IgM).
The degree of activity of the infectious process can be assessed based on the result of a quantitative polymerase chain reaction (PCR). This analysis allows you to detect the DNA of the virus, as well as to count the number of viral copies per unit volume of blood.
To assess the functional state of the liver, as well as monitor the dynamics of the disease, the following laboratory tests are regularly performed:
- blood chemistry;
- coagulogram;
- general analysis of blood and urine.

Hepatitis B virus is found in blood and body fluids
Be sure to perform ultrasound of the liver in dynamics.
If indicated, a puncture biopsy of the liver is performed, followed by histological and cytological examination of the punctate.
Treatment
Acute hepatitis B
The acute form of the disease is the basis for hospitalization of the patient. The patient is recommended strict bed rest, drinking plenty of fluids and adherence to a sparing diet (table number 5 according to Pevzner).
Antiviral therapy is carried out with a combination of interferons and ribavirin. Dosages and duration of treatment are determined by the doctor individually in each case.
To reduce the severity of intoxication syndrome, intravenous infusion of glucose solutions, crystalloids, potassium preparations is performed. Carrying out vitamin therapy is shown.

Acute hepatitis B is treated in a hospital using drip infusion of glucose and potassium preparations
In order to eliminate spasm of the biliary tract, antispasmodics are prescribed. When symptoms of cholestasis appear, ursodeoxycholic acid (UDCA) preparations must be included in the therapy regimen.
Chronic hepatitis B
Therapy of chronic hepatitis B is carried out with antiviral drugs and has the following goals:
- slowing down or completely stopping the progression of the disease;
- suppression of viral replication;
- elimination of fibrotic and inflammatory changes in liver tissue;
- preventing the development of primary liver cancer and cirrhosis.

For chronic hepatitis B, the doctor prescribes antiviral drugs
Currently, there is no single generally accepted standard for the treatment of viral hepatitis B. When choosing a therapy, the doctor takes into account all the factors that affect both the course of the disease and the general condition of the patient.
Possible complications and consequences
The most dangerous complication of hepatitis B is hepatic coma (hepatgia, acute liver failure). It arises as a result of massive death of hepatocytes, leading to significant violations of liver function, and is accompanied by a high mortality rate.
Against the background of hepatic coma, the addition of a secondary infection with the development of sepsis is often observed. In addition, hepatargia often leads to the development of acute nephrotic syndrome.
Hemorrhagic syndrome can cause internal bleeding, sometimes severe, life-threatening.
The main complication of the chronic form of viral hepatitis B is the formation of liver cirrhosis.
Forecast
Acute viral hepatitis B is rarely fatal. The prognosis worsens with mixed infection with hepatitis C and D viruses, the presence of concomitant chronic diseases of the hepatobiliary system, and fulminant course of the disease.
In the chronic form of hepatitis B, patients die several decades after the onset of the disease as a result of the development of primary cancer or cirrhosis of the liver.
Prevention
General measures to prevent infection with viral hepatitis B include:
- use of disposable medical instruments;
- careful control of the sterility of reusable instruments;
- performing blood transfusions only if there are strict indications;
- removal from donation of people who have had any form of hepatitis;
- using only individual personal hygiene items (toothbrushes, razors, manicure tools);
- refusal to use drugs;
- safe sex.
Vaccination is recommended for people at increased risk of hepatitis B infection. Immunity after vaccination lasts about 15 years, then revaccination is necessary to maintain it.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!






