- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Congenital hypothyroidism
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
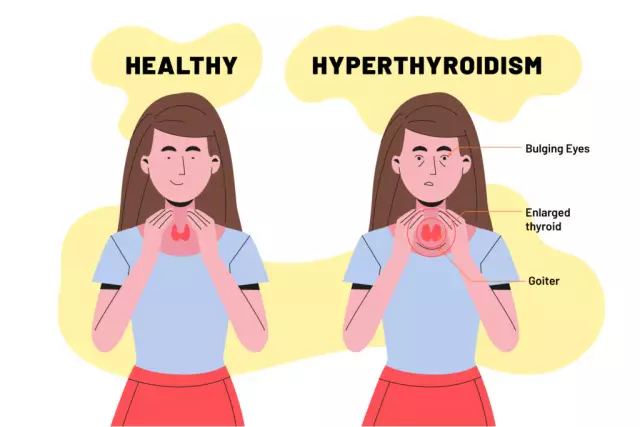
Congenital hypothyroidism is a group of diseases of various etiologies, manifested by congenital insufficiency of the production of thyroid hormones by the thyroid gland. The disease occurs with a frequency of 1 case per 5000 newborns, in boys - 2.5-3 times less often than in girls.
Lack of thyroid hormones has a negative effect on the development of the central nervous system. If congenital hypothyroidism is not detected in a timely manner and treatment is not started, the child develops mental impairment of varying severity. Therefore, in many countries, newborns are screened for hypothyroidism. Since 1997, screening has been carried out in all maternity hospitals in Russia.

Long-term physiological jaundice is one of the signs of congenital hypothyroidism
Causes and risk factors
In 80-90% of cases, congenital hypothyroidism is caused by malformations of the thyroid gland: for example, hypoplasia, dystopia (displacement) in the sublingual or retrosternal space.
The main risk factors for the formation of congenital hypothyroidism:
- lack of iodine in the body of a pregnant woman;
- exposure to ionizing radiation;
- toxic effects on the developing fetus of chemicals, including some medicines;
- infectious and autoimmune diseases of a pregnant woman.

Lack of iodine in a pregnant woman's body can lead to congenital hypothyroidism in a child
In about 2% of cases, thyroid abnormalities are caused by mutations in the PAX8, FOXE1, TITF2, TITF1 genes. With congenital hypothyroidism caused by genetic factors, other developmental anomalies are often observed in a child:
- non-closure of the hard palate (cleft palate);
- non-closure of the upper lip (cleft lip);
- congenital heart defects.
In 5% of cases, the cause of congenital hypothyroidism is hereditary diseases that lead to a violation of the secretion of thyroid hormones or disrupt their interaction with each other. Such diseases include Pendred's syndrome, defects in thyroid hormones and iodine organification. They are inherited in an autosomal recessive manner (both parents must be carriers of the defective genes).
In other cases, congenital hypothyroidism develops as a result of lesions of the hypothalamic-pituitary system due to:
- pituitary aplasia;
- asphyxia of the newborn;
- birth trauma;
- tumor processes;
- developmental anomalies of the brain.
The clinical picture of congenital hypothyroidism can be caused by a syndrome of resistance: in some hereditary diseases, the thyroid gland secretes a sufficient amount of thyroid hormones, but the target organs lose their sensitivity to them.
Forms of the disease
Depending on the reasons underlying the development of the disease, the following forms of congenital hypothyroidism are distinguished:
- thyrogenic, or primary - occurs as a result of pathological changes in the thyroid gland;
- secondary - the basis of its development is a deficiency of TSH (thyroid-stimulating hormone) associated with dysfunction of the adenohypophysis;
- tertiary - the reason is a deficiency of thyroliberin (hypothalamic hormone);
- peripheral. The mechanism of its development is associated with the absence of receptors for thyroid hormones in tropic tissues or their defect. Also, the cause of this form of congenital hypothyroidism can be a violation of the process of converting T4 (thyroxine) to T3 (triiodothyronine).
Depending on the effectiveness of the treatment, congenital hypothyroidism is divided:
- on compensated - there are no clinical symptoms of the disease, the concentration in blood plasma of T4, T3, TSH corresponds to the norm;
- to decompensated - laboratory and clinical manifestations of hypothyroidism persist, despite ongoing therapy.
According to the duration of the flow, two forms are distinguished:
- Transient. Lack of thyroid function in a child develops under the influence of maternal antibodies to TSH circulating in his blood. This form of the disease lasts from 7 to 30 days.
- Permanent. Hormone replacement therapy should be used for life.
According to the level of T4 in blood plasma and the intensity of the severity of clinical signs, congenital hypothyroidism can be:
- latent (subclinical);
- manifest;
- complicated.
Clinical manifestations in latent hypothyroidism are usually absent or nonspecific. Blood tests show elevated TSH levels with normal T4 levels.

Latent hypothyroidism is characterized by elevated TSH levels with normal T4
Complicated hypothyroidism is accompanied by the addition of other diseases (cretinism, polyserositis, heart failure). This form proceeds with a sharp deficiency of thyroxine at a very high level of thyroid-stimulating hormone.
Symptoms
Congenital hypothyroidism manifests itself at different ages - depending on the severity of the disease and its form. So, with aplasia of the thyroid gland or pronounced hypoplasia, the symptoms of hypothyroidism become clearly visible already in the first week of a child's life. Minor hypoplasia and dystopia manifest clinically after one year of age.
The main signs of congenital hypothyroidism:
- immaturity of a newborn born after 38 weeks of gestation;
- delay in the discharge of meconium;
- large fetus (birth weight exceeds 4 kg);
- long-term physiological jaundice;
- muscle atony;
- episodes of apnea (respiratory arrest) during feeding;
- hyporeflexia;
- flatulence;
- frequent regurgitation;
- a tendency to constipation;
- an increase in the size of the tongue (macroglossia);
- apathy;
- slow weight gain;
- swelling of the genitals and extremities;
- coldness of the skin to the touch;
- dysplasia of the hip joints;
- enlarged fontanelles.

Babies with congenital hypothyroidism are usually born large, weighing more than 4 kg
With the primary form of congenital hypothyroidism and the absence of treatment, the severity of the symptoms of the disease increases. The skin becomes dry and hardened, becoming an icteric gray. Myxedema develops (edema of the subcutaneous tissue and skin). Sweat separation is reduced. Hair and nail plates atrophy. Voice changes (becomes rough, hoarse and low). There are signs of delayed psychomotor development. If treatment is not started, then mental deficiency (oligophrenia) is formed.
The clinical picture of the central forms (secondary, tertiary) of congenital hypothyroidism is usually indistinct. The disease is often combined with a deficiency of other homones (follicle-stimulating, luteinizing, somatotropic), anomalies in the structure of the facial skull.
Diagnostics
Currently, the diagnosis of congenital hypothyroidism is based primarily on the results of neonatal screening. On the 4th-5th day of life, a few drops of blood are taken from a child and applied to filter paper, which is transferred to the laboratory to determine the concentration of TSH. The diagnosis of congenital hypothyroidism is considered confirmed when the concentration of TSH in the test sample exceeds 100 mU / L.

Congenital hypothyroidism is diagnosed based on a blood test for hormone levels
If the TSH content in a dry blood spot is higher than 20 mU / l, then the result is regarded as doubtful and the analysis is repeated. When a similar result is repeated, the determination of free T4 and TSH in the blood serum is shown.
Treatment
Treatment of congenital hypothyroidism should begin as soon as the diagnosis is made. Hormone replacement therapy is carried out for life with synthetic analogues of thyroid hormones. The dosage is selected individually in each case. If necessary, the doctor may additionally prescribe symptomatic remedies, multivitamins to the sick child. To assess the effectiveness of the treatment, the concentration in serum of T4 and TSH is determined.
Possible complications and consequences
If untreated, congenital hypothyroidism is complicated by damage to the central nervous system with the formation of oligophrenia.
With a deficiency of the thyroid gland, the immune system suffers, therefore, children with congenital hypothyroidism are prone to colds and other infectious diseases, which often become protracted and chronic.

Children with congenital hypothyroidism are prone to frequent colds and infections
The most dangerous complication of hypothyroidism is myxedema (hypothyroid) coma. It can be triggered by hypothermia, trauma, infectious diseases.
Forecast
In congenital hypothyroidism, the prognosis largely depends on the time of initiation of hormone replacement therapy. If it is started in the first months of life, then the psychophysical development of the child and his intellect do not suffer. When starting therapy at the age of 3-6 months, it is possible to stop further lag in psychomotor development. However, the already existing intellectual disabilities will remain for life.
Prevention
Prevention of congenital hypothyroidism includes:
- prevention of iodine deficiency in a pregnant woman;
- medical and genetic counseling for married couples at the stage of pregnancy planning, especially if one of the parents or someone from close relatives suffers from thyroid pathology;
- antenatal protection of the fetus.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!