- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Epidermolysis bullosa
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Epidermolysis bullosa is a large group of hereditary diseases that are characterized by the formation of blisters on the mucous membranes and skin (spontaneous or under the influence of minor traumatic effects). The incidence rate of epidermolysis bullosa is 1 to 3 cases per 100,000 population.
Attention! Photo of shocking content.
Click on the link to view.
Causes and risk factors
Depending on the type of disease epidermolysis bullosa is inherited either in an autosomal dominant or autosomal recessive manner. Mutations can be localized in more than 10 genes. These mutations impair the synthesis of protein molecules that provide skin elasticity (collagen, keratin, etc.).
Forms of the disease
Depending on the localization of the blisters, the following forms of epidermolysis bullosa are distinguished:
- Simple. The pathological process does not affect the lower layers of the skin. The disease is characterized by the formation of blisters in the mouth, thickening of the skin of the soles and palms. Bursting blisters heal without scarring.
- Border. Bubbles form in the area of the dermo-epidermal junction. In severe cases, they are formed in the organs of the genitourinary system, intestines and esophagus. Death is possible.
- Dystrophic. Clinical manifestations differ depending on the type of inheritance. Diseases with a recessive mode of inheritance are characterized by blistering in the esophagus, fusion of fingers and toes, and an increased risk of skin cancer. Diseases with a dominant type of inheritance are manifested by the appearance of blisters on the skin in the elbow and knee joints, on the mucous membranes.
- Malignant. Immediately after birth, a generalized hemorrhagic rash appears on the baby's skin and mucous membranes. After opening the bubbles, long-term non-healing erosion forms in their place. The accession of a secondary pyogenic infection causes the development of sepsis and the death of the newborn.

Microstructure of a skin sample of a patient with epidermolysis bullosa
Symptoms
Clinical manifestations of epidermolysis bullosa:
- easy trauma to the skin;
- milia (small white acne);
- blisters and erosion on the skin and mucous membranes;
- absence or thickening of the nail plates;
- thickening of the skin of the palms and soles;
- atrophic scars at the site of erosion healing;
- disorders of skin pigmentation;
- lack or thinning of hair;
- violation of sweating (increase or decrease);
- fusion of fingers and toes;
- susceptibility to caries;
- frequent vomiting;
- dysphagia;
- a tendency to constipation;
- slow growth;
- low body weight.
Children with epidermolysis bullosa are often referred to as “butterfly babies” because of the fragility of their skin.

Butterfly baby Lisa Kunigel - even a light touch on the skin causes blisters
Diagnostics
Diagnosis of epidermolysis bullosa can be prenatal (before birth) and postnatal (after birth).
Prenatal diagnosis is based on genetic analysis of the amniotic fluid obtained during amniocentesis performed after the 17th week of pregnancy.
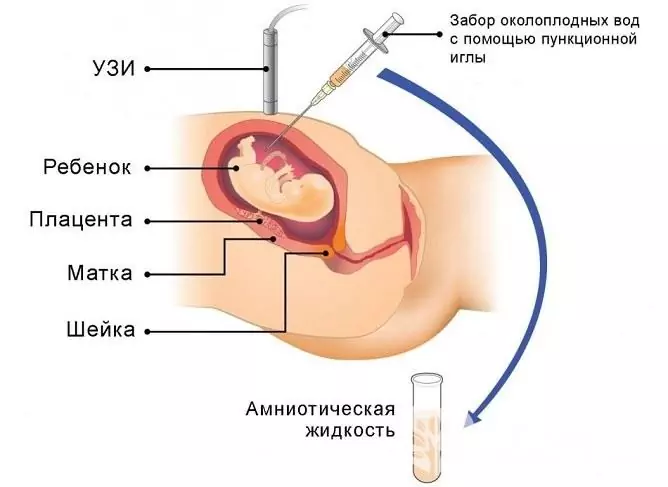
Epidermolysis bullosa can be diagnosed before childbirth by examining the amniotic fluid
Postnatal is done by electron microscopy (TEM) and immunofluorescence genetic mapping (IAM). This requires skin samples from undamaged and damaged areas; they are obtained by biopsy.
DNA analysis plays an important role in the diagnosis of epidermolysis bullosa. It allows you to identify the localization of the mutated gene, as well as determine the type of inheritance of the disease.
Treatment
There are no specific methods of therapy for epidermolysis bullosa, the treatment is symptomatic. The main efforts are aimed at preventing injury to the skin, as well as preventing the addition of a secondary pyogenic infection.
It is important to carry out local treatment correctly. The resulting bubbles, in compliance with the rules of asepsis and antiseptics, are pierced from both sides, and the “lid” of the bubble is lubricated with a solution of methylene blue or brilliant green. Ointments with antibiotics or corticosteroids are applied to the surface of the erosion. Ultraviolet irradiation of the skin has a good healing effect.

Treatment of epidermolysis bullosa symptomatic
In severe epidermolysis bullosa, local therapy is supplemented by systemic use of corticosteroids.
Possible complications and consequences
The main complication of epidermolysis bullosa is suppuration of the eroded surface as a result of the attachment of a secondary infection. With reduced immunity, the spread of purulent infection is possible (up to the development of sepsis).
Forecast
The prognosis for epidermolysis bullosa is largely determined by the form of the disease. It is most favorable for a simple form.
Prevention
Since epidermolysis bullosa is a hereditary disease, there are no specific measures for its prevention. If there have been cases of this disease in the family, then genetic counseling is recommended for a married couple at the stage of pregnancy planning. In the second trimester of pregnancy, amniocentesis is shown, followed by histological and genetic analysis of the resulting punctate. If genetic mutations characteristic of severe forms of epidermolysis bullosa (malignant, dystrophic) are detected in the fetus, the couple is recommended to terminate the pregnancy for medical reasons.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!






