- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Arachnoiditis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Arachnoiditis is a serous (non-purulent) inflammation of the arachnoid membrane of the spinal cord or brain.
The arachnoid membrane is a thin lining of connective tissue located between the outer hard and inner pia mater. Between the arachnoid and soft membranes, the subarachnoid (subarachnoid) space contains cerebrospinal fluid - cerebrospinal fluid, which maintains the constancy of the internal environment of the brain, protects it from injury and ensures the physiological course of metabolic processes.
With arachnoiditis, the arachnoid membrane thickens, loses its transparency, acquires a whitish-gray color. Adhesions and cysts are formed between it and the soft shell, disrupting the movement of the cerebrospinal fluid in the subarachnoid space. Restriction of the circulation of cerebrospinal fluid leads to an increase in intracranial pressure, displacement and increase in the ventricles of the brain.

Arachnoiditis - serous inflammation of the arachnoid membrane of the brain or spinal cord
The arachnoid membrane does not have its own blood vessels, therefore, its isolated inflammation is formally impossible; the inflammatory process is a consequence of the transition of pathology from neighboring membranes. In this regard, recently the legality of using the term "arachnoiditis" in practical medicine has been questioned: some authors suggest considering arachnoiditis as a type of serous meningitis.
Synonym: leptomeningitis, adhesive meningopathy.
Causes and risk factors
Arachnoiditis refers to polyetiological diseases, that is, it can appear under the influence of various factors.
The leading role in the development of arachnoiditis is assigned to autoimmune (autoallergic) reactions in relation to the cells of the pia mater, choroid plexus and tissue lining the cerebral ventricles, arising independently or as a result of inflammatory processes.
Most often, arachnoiditis develops as a result of the following diseases:
- acute infections (flu, measles, scarlet fever, etc.);
- rheumatism;
- tonsillitis (inflammation of the tonsils);
- inflammation of the paranasal sinuses (sinusitis, frontal sinusitis, ethmoiditis);
- inflammation of the middle ear;
- inflammation of the tissues or membranes of the brain (meningitis, encephalitis).
Risk factors:
- past trauma (post-traumatic arachnoiditis);
- chronic intoxication (alcohol, heavy metal salts);
- exposure to occupational hazards;
- chronic inflammatory processes of the ENT organs;
- hard physical labor in adverse climatic conditions.
The disease usually develops at a young age (up to 40 years), more often in children and those exposed to risk factors. Men get sick 2 times more often than women. It is not possible to find out the cause of the disease in 10-15% of patients.
Forms of the disease
Depending on the causative factor, arachnoiditis is:
- true (autoimmune);
- residual (secondary), arising as a complication of the transferred diseases.
For the involvement of the central nervous system:
- cerebral (brain involved);
- spinal (the spinal cord is involved).
According to the predominant localization of the inflammatory process in the brain:
- convexital (on the convex surface of the cerebral hemispheres);
- basilar, or basal (optic-chiasmal or interpeduncular);
- posterior cranial fossa (cerebellopontine angle or cisterna magna).
By the nature of the flow:
- subacute;
- chronic.
In terms of prevalence, arachnoiditis can be diffuse and limited.
By pathomorphological characteristics:
- adhesive;
- cystic;
- adhesive cystic.
Symptoms
Arachnoiditis proceeds, as a rule, subacutely, with a transition to a chronic form.
The manifestations of the disease are formed from general cerebral and local symptoms, presented in various ratios, depending on the localization of the inflammatory process.
At the heart of the development of cerebral symptoms are the phenomena of intracranial hypertension and inflammation of the inner membrane of the ventricles of the brain:
- a bursting headache, often in the morning, soreness when moving the eyeballs, physical exertion, coughing, may be accompanied by bouts of nausea;
- episodes of dizziness;
- noise, ringing in the ears;
- intolerance to exposure to excessive stimuli (bright light, loud sounds);
- meteosensitivity.

With arachnoiditis, severe bursting headaches occur in the morning
Arachnoiditis is characterized by liquorodynamic crises (acute disturbances in the circulation of cerebrospinal fluid), which are manifested by an increase in cerebral symptoms. Depending on the frequency, crises are distinguished as rare (1 time per month or less), medium frequency (2-4 times a month), frequent (weekly, sometimes several times a week). The severity of CSF crises varies from mild to severe.
Local manifestations of arachnoiditis are specific for a specific localization of the pathological process.
Focal symptoms of convexital inflammation:
- trembling and tension in the limbs;
- change in gait;
- limitation of mobility in an individual limb or half of the body;
- decreased sensitivity;
- epileptic and Jacksonian seizures.
Local symptoms of basilar arachnoiditis (the most common is optic-chiasmal arachnoiditis):
- the appearance of extraneous images before the eyes;
- progressive decrease in visual acuity (more often bilateral, lasting up to six months);
- concentric (less often - bitemporal) loss of visual fields;
- unilateral or bilateral central scotomas.
Local symptoms of arachnoid lesion in the posterior cranial fossa:
- instability and unsteadiness of gait;
- the inability to produce combined synchronous movements;
- loss of the ability to quickly perform opposite movements (flexion and extension, turn inward and outward);
- instability in the Romberg position;
- trembling of the eyeballs;
- violation of the finger test;
- paresis of the cranial nerves (more often - the abducens, facial, auditory and glossopharyngeal).

Unsteadiness and unsteadiness of gait occurs with arachnoiditis of the posterior cranial fossa
In addition to the specific symptoms of the disease, manifestations of asthenic syndrome reach significant severity:
- unmotivated general weakness;
- violation of the "sleep - wakefulness" regime (sleepiness during the day and insomnia at night);
- memory impairment, decreased concentration;
- decreased performance;
- increased fatigue;
- emotional lability.
Diagnostics
Inflammation of the arachnoid membrane of the brain is diagnosed by comparing the clinical picture of the disease and data from additional studies:
- plain x-ray of the skull (signs of intracranial hypertension);
- electroencephalography (change in bioelectric parameters);
- studies of cerebrospinal fluid (a moderately increased number of lymphocytes, sometimes a small protein-cell dissociation, fluid leakage under increased pressure);
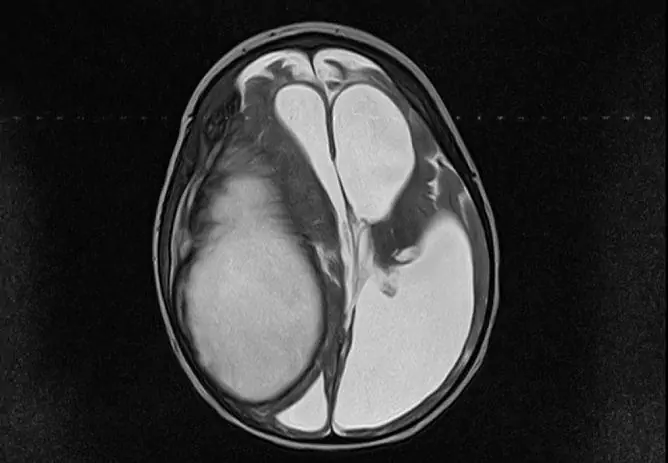
- tomography (computer or magnetic resonance imaging) of the brain (expansion of the subarachnoid space, ventricles and cisterns of the brain, sometimes cysts in the intrathecal space, adhesive and atrophic processes in the absence of focal changes in the brain substance).

To diagnose arachnoiditis, an X-ray of the skull, CT, MRI are performed
Treatment
Complex therapy of arachnoiditis includes:
- antibacterial agents to eliminate the source of infection (otitis media, tonsillitis, sinusitis, etc.);
- desensitizing and antihistamines;
- absorbable agents;
- nootropic drugs;
- metabolites;
- drugs that reduce intracranial pressure (diuretics);
- anticonvulsants (if necessary);
- symptomatic therapy (according to indications).
Possible complications and consequences
Arachnoiditis can have the following formidable complications:
- persistent hydrocephalus;
- progressive deterioration of vision, up to complete loss;
- epileptic seizures;
- paralysis, paresis;
- cerebellar disorders.
Forecast
Life prognosis is usually good.
The prognosis for work activity is unfavorable with a progressive crisis, epileptic seizures, and progressive visual impairment. Patients are recognized as invalids of groups I - III, depending on the severity of the condition.
Patients with arachnoiditis are contraindicated to work in adverse meteorological conditions, in noisy rooms, in contact with toxic substances and in conditions of altered atmospheric pressure, as well as work associated with constant vibration and changes in head position.
Prevention
For prevention purposes, you need:
- timely sanitation of foci of chronic infection (carious teeth, chronic sinusitis, tonsillitis, etc.);
- full-fledged follow-up treatment of infectious and inflammatory diseases;
- control of the functional state of brain structures after traumatic brain injury.
YouTube video related to the article:

Olesya Smolnyakova Therapy, clinical pharmacology and pharmacotherapy About the author
Education: higher, 2004 (GOU VPO "Kursk State Medical University"), specialty "General Medicine", qualification "Doctor". 2008-2012 - Postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty "Pharmacology, Clinical Pharmacology"). 2014-2015 - professional retraining, specialty "Management in education", FSBEI HPE "KSU".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!