- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Esophageal atresia
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
Esophageal atresia is a congenital malformation in which part of the esophagus is missing in the newborn, which causes esophageal obstruction. This pathology requires early surgical intervention, otherwise it leads to the death of the child.

Types of esophageal atresia
Esophageal atresia occurs with a frequency of 1 to 4 cases per 1000 newborns (with the same frequency in children of both sexes). It is often combined with other developmental anomalies, such as:
- malformations of the extremities, including dysplasia of the radius;
- choanal atresia;
- atresia of the anus;
- tracheoesophageal fistula;
- malformation of the spinal column (VACTERL syndrome, or VATER);
- kidney abnormalities;
- heart defects;
- agenesis of the gallbladder;
- pyloric stenosis.
In about 5% of cases, esophageal atresia is associated with certain chromosomal abnormalities (for example, Down syndrome, Edwards or Patau syndrome). One third of newborns with esophageal atresia are born prematurely or have signs of intrauterine growth retardation. Pregnancy by a fetus with an abnormality in the development of the esophagus is often accompanied by the threat of early miscarriage or polyhydramnios in the II and III trimesters.
Causes and risk factors
The formation of esophageal atresia occurs at 4-12 weeks of gestation. In early embryogenesis, the trachea and esophagus communicate with each other, as they develop from the cranial section of the primary intestine. Violation of the processes of recanalization, lacing of the esophagus from the respiratory tube, the growth rate of the trachea and esophagus lead to the appearance of esophageal atresia.

In the course of prenatal diagnosis, esophageal atresia can be suspected with polyhydramnios, a stomach that is too small or absent.
Esophageal atresia occurs due to negative factors affecting the body of a pregnant woman:
- chronic intoxication;
- alcoholism, drug addiction;
- infectious diseases (influenza, rubella, cytomegalovirus);
- taking medications with teratogenic effects;
- ionizing radiation.
Forms of the disease
Esophageal atresia is of two forms:
- Fistulous. It is characterized by the presence of communication between the trachea and the esophagus (tracheoesophageal fistula).
- Isolated. With her, the trachea and esophagus do not communicate with each other.
Fistulous forms of esophageal atresia are much more common, which, in turn, are of several types:
- fistulous atresia of the trachea and both ends of the esophagus;
- fistulous atresia of the trachea and the proximal segment of the esophagus;
- fistulous atresia of the trachea and distal segment of the esophagus.
Sometimes the child has a tracheoesophageal fistula, but without esophageal atresia.
The most severe form of esophageal atresia is aplasia, that is, its complete absence.
The most typical place of localization of esophageal atresia is the tracheal bifurcation area. The part of the esophagus that is not connected to the trachea by the fistulous tract ends blindly. The isolated form of the disease is characterized by the presence of two blindly ending sections of the esophagus, which either go behind each other or touch each other.
Symptoms
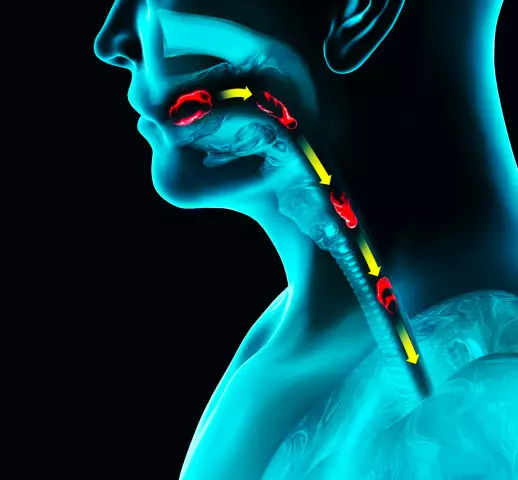
The clinical picture of esophageal atresia manifests itself in newborns already in the first hours of life. The first symptom is false hypersalivation, which is characterized by the discharge of a large amount of frothy saliva from the child's mouth and nose. Some of the saliva and mucus passes from the esophagus into the trachea. This leads to impaired respiratory function and the appearance of shortness of breath, tachypnea, paroxysmal cough, wheezing, cyanosis and asphyxia.
Suction of mucus from the nasal cavity, mouth and pharynx, as well as tracheal aspiration, eliminate the above symptoms, but after a while they reappear.

With atresia of the esophagus, saliva, mucus, food enters the respiratory tract
When feeding a newborn, esophageal atresia is manifested by the following symptoms:
- instant regurgitation;
- vomiting of unchanged milk;
- severe paroxysmal cough;
- suffocation;
- acrocyanosis;
- bloating.
Diagnostics
Diagnosis of esophageal atresia should be carried out as soon as possible, before the development of aspiration pneumonia or water-electrolyte disorders.
If there is a suspicion of obstruction, the esophagus is immediately probed through the nasal cavity with a soft rubber catheter. With atresia, it is impossible to pass the probe into the gastric cavity: if you continue the introduction, despite a noticeable obstacle, the probe is wrapped and its end comes out.
To confirm the diagnosis, an Elephant test is performed. It consists in introducing air into the esophagus through a catheter using a syringe. With atresia, air with a characteristic noise comes out of the nasopharynx.
To establish the type of esophageal atresia, bronchoscopy and esophagoscopy are performed. Radiography with contrasting with barium suspension in this pathology is often accompanied by the development of respiratory complications that can cause the death of an infant, therefore such a study is performed extremely rarely and only for strict indications.

X-ray of esophageal atresia in a child
Esophageal atresia requires differential diagnosis with the following pathologies:
- cleft larynx;
- isolated tracheoesophageal fistula;
- congenital pyloric stenosis;
- esophagus spasm;
- esophageal stenosis.
Treatment
Esophageal atresia is an indication for emergency surgery: the operation must be performed within the first 36 hours of a newborn's life. Preoperative preparation begins in a maternity hospital. It includes:
- giving the baby a posture in which the ingress of acidic gastric contents into the respiratory tract through the distal tracheoesophageal fistula is eliminated;
- exclusion of oral feeding;
- repeated and frequent aspiration of mucus from the respiratory tract;
- constant inhalation of humidified oxygen;
- antibacterial therapy;
- correction of water and electrolyte disturbances.
Possible complications and consequences
Recurrent vomiting leads to depletion and the development of severe water-electrolyte disorders.
The ingestion of food and mucus into the respiratory tract causes aspiration pneumonia, manifested by fever and increasing symptoms of acute respiratory failure, against which a fatal outcome can occur.
In the long-term period after surgical treatment of esophageal atresia, 40% of children develop cicatricial esophageal stenosis, which requires bougienage of the anastomosis.
Forecast
The prognosis for esophageal atresia depends on many factors. With an isolated form of the disease and surgical intervention, 90-100% of children survive until complications appear. With prematurity or concomitant malformations, the survival rate of children with esophageal atresia does not exceed 30-50%.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!