- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Impaired glucose tolerance
The content of the article:
- Causes and risk factors
- Symptoms
- Features of impaired glucose tolerance in children
-
Diagnostics
- Contraindications to the glucose tolerance test
- Test preparation
- Testing
- Interpretation of sample results
- Additional diagnostics
-
Treatment of impaired glucose tolerance
- Diet
- Other recommendations
- Possible complications and consequences
- Forecast
- Prevention
- Video
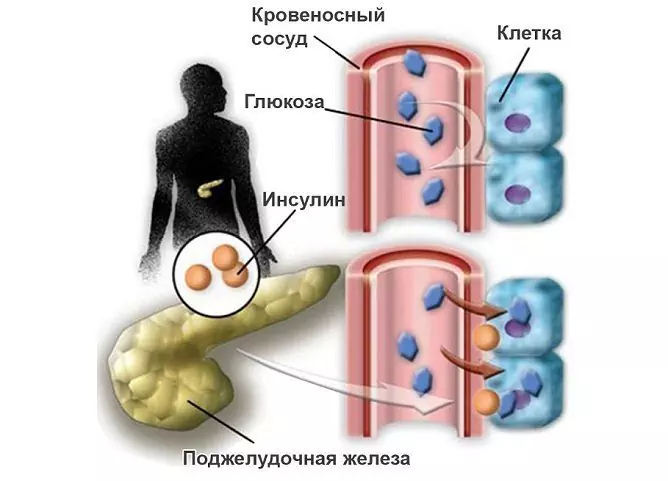
Impaired glucose tolerance (IGT) is a form of latent diabetes characterized by the absence of clinical signs of diabetes with an inadequate increase in blood sugar and a slow decrease in blood sugar under the influence of various reasons (usually after eating). This is a high risk condition for the development of clinically significant diabetes mellitus in the future. In addition, people with impaired glucose tolerance usually have more severe comorbidities.
Timely detection of such a violation of carbohydrate metabolism allows you to take measures in order to avoid the development of diabetes mellitus, or, at least, significantly delay its occurrence. Diagnosis is not difficult; an oral glucose tolerance test is sufficient.

Synonyms: prediabetes, asymptomatic diabetes, subclinical diabetes, latent diabetes, latent diabetes.
In the International Classification of Diseases 10 edition (ICD-10), the disease has the code R73.0.
Causes and risk factors
The origin of the carbohydrate metabolic disorder is reflected in the classification of diabetes mellitus published by the World Health Organization in 1999. Glucose tolerance can be reduced for the following reasons:
| Etiological factor | Decoding |
| Genetic disorders |
Dysfunction of β-cells (insulin-producing cells of the pancreas); · Violation of insulin absorption; · Genetically determined destruction of β-cells; · Genetically determined insulin resistance. |
| Endocrinopathies | Itsenko-Cushing's syndrome, thyrotoxicosis, pheochromocytoma, acromegaly, etc. |
| Obesity | BMI (body mass index) ≥ 25 kg / m 2 |
| Viral infections |
· Epstein-Barr virus; · Cytomegalovirus; · Mumps virus. |
| Diabetogenic drugs and other chemicals | Glucocorticoids, α-adrenergic receptor agonists, thiazides, α-interferon, pentamidine, etc. |
| Genetic and chromosomal syndromes accompanied by impaired glucose tolerance | Down syndrome, Shereshevsky-Turner, Lawrence-Moon, Wolfram, Huntington's chorea, etc. |
| Diseases of the exocrine pancreatic apparatus | Pancreatitis, cystic fibrosis, some neoplasias. |
The factors that contribute to the development of prediabetes are many and varied. These include:
- overweight;
- a family history of diabetes mellitus;
- sedentary lifestyle;
- age over 45;
- arterial hypertension;
- deviations from the norm in the content of HDL cholesterol in the blood;
- high levels of triglycerides in the blood;
- some metabolic disorders (gout, hyperuricemia, atherosclerosis, metabolic syndrome);
- chronic diseases of the liver, kidneys, cardiovascular system;
- furunculosis;
- periodontal disease;
- a history of gestational diabetes;
- miscarriage, pregnancy that ended in stillbirth, premature birth, history of excessively large fetus;
- severe stress, major surgery, a history of serious illness.
All people with these conditions should have a regular glucose tolerance test.
Symptoms
There are no clinical manifestations of impaired glucose tolerance - it is for this reason that it is called asymptomatic, or subclinical diabetes. The condition can only be detected by performing a glucose tolerance test as part of a prophylactic examination or diagnostic examination for another reason.
However, experts tend to consider some signs as potentially indicating a possible impairment of glucose tolerance, in particular:
- susceptibility to skin diseases (furunculosis, fungal infection, pyoderma, pruritus), alopecia:
- bleeding gums, periodontal disease;
- intestinal dysbiosis, irritable bowel syndrome, pancreatic dysfunction;
- disorders of the menstrual cycle in women, sexual dysfunction in men, candidiasis of the genitourinary system;
- angioneuropathy, retinopathy, obliterating endarteritis.
Features of impaired glucose tolerance in children
Despite the fact that in children and adolescents, impaired glucose tolerance usually develops under the influence of a stress factor and is transient, it, being confirmed to avoid a false-positive result, indicates the presence of type 1 diabetes mellitus (juvenile, insulin-dependent diabetes). In this case, impaired glucose tolerance is considered not as prediabetes, but as a stage in the development of type 1 diabetes mellitus, which precedes its manifestation. In contrast to latent diabetes in adults, in children, prediabetes is irreversible and requires constant monitoring of blood glucose levels in order to initiate insulin therapy in a timely manner.
Diagnostics
The method of diagnosing impaired glucose tolerance is a special test for glucose tolerance, since the usual test that determines the level of glucose in the blood will not deviate from the norm at the stage of pre-diabetes. A glucose tolerance test is a safe, inexpensive, and highly informative method.
During the test, the adequacy of endogenous insulin secretion is determined, which is manifested in the body's ability to maintain normal blood glucose levels under stressful conditions of drinking glucose.
Contraindications to the glucose tolerance test
- the blood glucose level is higher than the diagnostic threshold of diabetes mellitus (7 mmol / l);
- the glucose level at any time of the day, regardless of food intake, corresponds to 11.1 mmol / l and above;
- recent surgery, myocardial infarction;
- postpartum period.
Test preparation
For three days before the study, the patient must adhere to his usual physical activity and a diet that includes at least 150 g of carbohydrates per day. The last meal should take place no later than 12 hours before the start of the test. 15 minutes before the start of the test and throughout its duration, the patient should be in a state of physical rest. This should not be preceded by stress, physical overload or illness.
Testing
During the test, the patient should be calm, sitting comfortably or lying down.
The test is performed in the morning on an empty stomach.
A blood sample is taken from a finger (capillary blood). Immediately after this, the patient is given a glucose solution to drink (75 g of dry glucose in 250 ml of water), to which a few drops of lemon juice or citric acid solution are sometimes added in order to avoid nausea and other unpleasant sensations. The exact amount of glucose is calculated based on 50 g / m2 of body surface, but not more than 75 g for adults, with obesity - at the rate of 1 g / kg of body weight, but not more than 100 g. The amount of glucose for children and adolescents is 1.75 g / kg body weight, but not more than 75 g.
After consuming glucose on an empty stomach, capillary blood is taken after 30, 60, 90, 120 minutes. During a preventive examination, the test can be carried out by a simplified method, when the first blood sampling is performed, as in the classical version, before the glucose load, and the second and last - after 120 minutes.
Interpretation of sample results
Normally, blood glucose levels rise immediately after a glucose load and then rapidly decrease. The initial glucose level should be less than 5.5 mmol / L, after 30, 60 and 90 minutes it should not exceed 11.1 mmol / L, and after 120 minutes it should be below 7.8 mmol / L.
If the fasting blood glucose exceeds 5.5 mmol / L, but below 6.1 mmol / L, and after 120 minutes is in the range of 7.8-11.1 mmol / L, a violation of glucose tolerance is diagnosed.
If the fasting blood glucose exceeds 6.1 mmol / L, and 120 minutes after a glucose load ≥ 11.1 mmol / L, diabetes is diagnosed.
If the fasting blood glucose level is in the range of 5.6-6.0 mmol / l, they speak of a violation of fasting glycemia, this condition indicates the existing risk of developing diabetes mellitus.
In people over 60 years old, 0.1 mmol / l is added to the obtained blood glucose levels every 10 years.
Quote: Studies by foreign endocrinologists show that 10% of people aged 60 and older have impaired glucose tolerance.
Additional diagnostics
An auxiliary diagnostic criterion for confirming the diagnosis of impaired glucose tolerance or diabetes mellitus is the determination of the level of glucose in urine collected after glucose load.
Another auxiliary method is the measurement of glycated hemoglobin (HbA1c) - an indirect indicator of the average concentration of glucose in the blood over a long period. Normally, the HbA1c index is 4-6%. At the same time, the detection of elevated HbA1c in people without clinical manifestations of diabetes mellitus requires a blood glucose test and a glucose tolerance test.
Treatment of impaired glucose tolerance
At the stage of pre-diabetes, to normalize the disturbed carbohydrate metabolism, it is sufficient to correct the lifestyle, which, however, should not be temporary, but lifelong.

At the pre-diabetes stage, the development of a clinically expressed disease can still be avoided
Diet
The main treatment for impaired glucose tolerance is diet. Its basic principles:
- Reducing the fat content in the diet to 40-50 g per day.
- Reducing salt intake to 6 g per day maximum.
- Reducing the consumption of simple carbohydrates (products made from white flour and butter dough, pastries, sugar, honey).
- Daily consumption of a small amount of complex carbohydrates (whole grain flour products, potatoes, cereals excluding semolina), evenly distributed over several meals.
- Preference for a dairy-plant diet (fresh and cooked vegetables, fruits and berries, dairy and fermented milk products should be included in the daily diet). Fermented milk products, in addition to their nutritional value, contribute to the prevention of intestinal dysbiosis, often accompanying disorders of carbohydrate metabolism.
- Refusal from alcoholic beverages.
- Fractional diet: 5-6 meals a day in small portions, observing equal time intervals between meals.
- In obesity, the daily caloric content (determined individually, taking into account gender, age, type of activity) of food should be reduced by 200-300 kcal until normal body weight is reached.
Other recommendations
- Quitting smoking and other bad habits.
- Avoiding hypodynamia, increasing physical activity. Requires daily physical activity without overwork.
- Regular monitoring of blood sugar levels.
- Normalization of work and rest regime, full night sleep.
- Refusal from heavy physical labor, night shifts.
- Observation by an endocrinologist with an annual examination, which includes a glucose tolerance test and determination of HbA1c.
Possible complications and consequences
The main complication of impaired glucose tolerance is the development of diabetes mellitus with all the consequences that this disease carries.
Forecast
According to available medical statistics, 10 years after the detection of impaired glucose tolerance in a third of patients, blood sugar levels return to normal, in a third they remain at the same level, and another third develops clinically expressed diabetes mellitus. The optimism of the prognosis depends on how seriously the patient treats medical recommendations for correcting his lifestyle.
Prevention
A measure of preventing the development of a pre-diabetic state is, first of all, maintaining a healthy lifestyle, which implies proper nutrition, regular and sufficient physical activity, a normal mode of work and rest, and stress resistance.
Secondary prevention includes the timely detection of a violation of carbohydrate metabolism (regular preventive examinations) and measures to eliminate it, including registration with a dispensary with an endocrinologist.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!