- Author Rachel Wainwright [email protected].
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Obstructive jaundice
The content of the article:
- The causes of obstructive jaundice
- Obstructive jaundice symptoms
- Diagnostics
- Obstructive jaundice treatment
- Diet for obstructive jaundice
- Prevention
- Possible complications
Obstructive jaundice is a clinical syndrome that develops as a result of a violation of the outflow of bile through the biliary tract into the duodenum and manifests itself as icteric staining of the skin and mucous membranes, pain in the right hypochondrium, dark urine, acholic feces, and an increase in the concentration of bilirubin in the blood serum.
Most often, obstructive jaundice develops as a complication of gallstone disease, but it can also be caused by other pathologies of the digestive tract. If medical care is not provided in a timely manner, this condition can provoke the development of liver failure and be fatal.

Source: pechenka.online
The causes of obstructive jaundice
The immediate cause of obstructive jaundice is obstruction (blockage) of the biliary tract. It can be partial or complete, which determines the severity of the clinical manifestations of the syndrome.
Obstructive jaundice can result from the following diseases:
- cholecystitis;
- cholangitis;
- cysts of the biliary tract;
- cholelithiasis;
- strictures or scars of the bile ducts;
- hepatitis, liver cirrhosis;
- pancreatitis;
- tumors of the liver, duodenum, stomach, or pancreas;
- parasitic invasions;
- Mirizzi syndrome;
- an increase in lymph nodes located in the area of the liver gate;
- surgical interventions on the biliary tract.
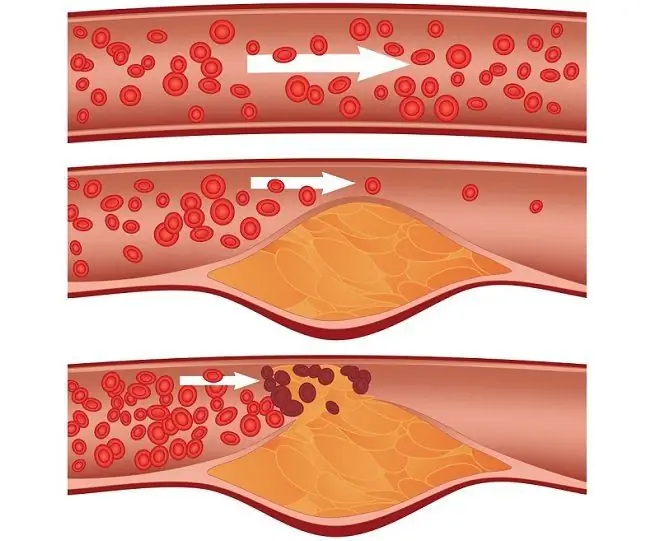
The pathological mechanism for the development of obstructive jaundice is complex. In most cases, it is based on an inflammatory process that affects the biliary tract. Against the background of inflammation, edema and thickening of the mucous membrane of the ducts occurs, which leads to a decrease in their lumen. By itself, this process disrupts the passage of bile. If at this moment even a small calculus enters the duct, the outflow of bile through it may completely stop altogether. Accumulating and stagnating in the bile ducts, bile promotes their expansion, destruction of hepatocytes, and the entry of bilirubin and bile acids into the systemic circulation. Bilirubin, which enters the bloodstream from the bile ducts, is not bound to proteins - this explains its high toxicity for cells and tissues of the body.

Source: pechen1.ru
Cessation of the flow of bile acids into the intestine disrupts the absorption of fats and fat-soluble vitamins (K, D, A, E). As a result, the process of blood coagulation is disrupted, hypoprothrombinemia develops.
Prolonged stagnation of bile in the intrahepatic ducts contributes to the pronounced destruction of hepatocytes, gradually leading to the formation of liver failure.
Factors that increase the risk of developing obstructive jaundice are:
- a sharp decrease in weight or, conversely, obesity;
- liver and pancreas infections;
- surgical interventions on the liver and biliary tract;
- injuries to the right upper quadrant of the abdomen.
Obstructive jaundice symptoms
Acute onset is rare, most often the clinical picture develops gradually. Usually, the symptoms of obstructive jaundice are preceded by inflammation of the biliary tract, the signs of which are:
- cramping pain in the right hypochondrium;
- increased body temperature;
- weakness;
- decreased appetite;
- headache.
Later, an icteric coloration of the skin and mucous membranes appears, which intensifies over time. As a result, the patient's skin becomes yellowish-greenish. Other signs of obstructive jaundice are dark coloration of urine, discoloration of feces, itching of the skin.

Source: cdn77.org
If the patient is not provided with medical care, then against the background of mass death of hepatocytes, liver functions are impaired, liver failure develops. Clinically, it is manifested by the following symptoms:
- increased fatigue;
- drowsiness;
- coagulopathic bleeding.
As the liver failure progresses, the patient's functioning of the brain, kidneys, heart, lungs is disrupted, that is, multiple organ failure develops, which is a prognostically unfavorable sign.
Diagnostics
A patient with obstructive jaundice is admitted to the department of gastroenterology or surgery. As part of the primary diagnosis, ultrasonography of the biliary tract and pancreas is performed. When detecting expansion of the intrahepatic bile ducts and common bile duct (bile duct), the presence of calculi, computed tomography of the biliary tract and magnetic resonance cholangiopancreatography can additionally be prescribed.

Source: infopechen.ru
Dynamic scintigraphy of the hepatobiliary system and percutaneous transhepatic cholangiography are performed to identify the degree of obstruction of the biliary tract, the peculiarities of the location of calculus and outflow of bile.
The most informative diagnostic method for obstructive jaundice is retrograde cholangiopancreatography. The method combines X-ray and endoscopic studies of the biliary tract. If, during the study, calculi located in the lumen of the common bile duct are found, they are removed (extracted), that is, the procedure from the diagnostic goes to the therapeutic. If a tumor that has caused obstructive jaundice is found, a biopsy is performed, followed by a histological analysis of the biopsy.
Laboratory research for obstructive jaundice includes the following studies:
- coagulogram (prothrombin time lengthening is detected);
- biochemical blood test (increased activity of transaminases, lipase, amylase, alkaline phosphatase, direct bilirubin level);
- a general blood test (an increase in the number of leukocytes, a shift in the leukocyte formula to the left, an increase in ESR, a decrease in the number of platelets and erythrocytes is possible);
- coprogram (there are no bile acids in the feces, fats are present in a significant amount).
Obstructive jaundice treatment
The main method of treating obstructive jaundice is surgical intervention, the purpose of which is to restore the outflow of bile into the duodenum. In order to stabilize the patient's condition, detoxification, infusion and antibacterial therapy is carried out. The following methods are used to temporarily improve the outflow of bile:
- choledochostomy - creating drainage by imposing an external fistula on the bile duct;
- cholecystostomy - the formation of an external fistula of the gallbladder;
- percutaneous puncture of the gallbladder;
- nasobiliary drainage (placing a catheter in the biliary tract during retrograde cholangiopancreatography).
If, despite the undertaken treatment of obstructive jaundice, the patient's condition does not improve, percutaneous transhepatic drainage of the bile ducts is indicated.
After stabilization of the patient's condition, the question of the next stage of treatment of obstructive jaundice is decided. Endoscopy methods are preferred because they are less traumatic. With tumor strictures and cicatricial stenosis, bougienage of the biliary tract is performed, followed by installation of stents in their lumen, i.e., endoscopic stenting of the common bile duct is performed. When the sphincter of Oddi is blocked by a stone, endoscopic balloon dilation is used.
In cases where endoscopic methods fail to remove the obstacle to the outflow of bile, they resort to traditional open abdominal surgery. In order to prevent leakage of bile into the abdominal cavity through the seams in the postoperative period, external drainage of the bile ducts according to Halstead is performed (installation of a polyvinyl chloride catheter in the cystic duct stump) or external drainage of the biliary tract according to Keru (installation of a special T-shaped tube in them).

Source: baumanki.net
Diet for obstructive jaundice
In the complex treatment of obstructive jaundice, therapeutic nutrition is of no small importance. In the preoperative period, the diet should ensure a decrease in the load on the liver cells, and after surgery, contribute to the early recovery of the body.
The patient is recommended to drink at least two liters of fluid per day, this contributes to the early elimination of bilirubin, thereby reducing its negative effect on the central nervous system, kidneys, and lungs.
The menu of patients in the preoperative period should include carbohydrate-rich drinks (glucose solution, compote, sweet weak tea). This allows you to meet the energy needs of the body and at the same time does not overload the liver, improves metabolic processes.
After performing surgery and improving the patient's condition, the diet is slowly expanded, gradually introducing fruit juices, milk porridge, and vegetable soups into the diet. Food should be taken in pureed form and at room temperature. With normal food tolerance, fish or meat dishes (steam or boiled) are included in the diet.
Fats in the diet are significantly limiting. With good tolerance, the patient can be given a very small amount of butter and vegetable oil. Animal fats are contraindicated.
After the patient's condition is steadily stabilized, it is allowed to include yesterday's or dried white bread, low-fat dairy products in the diet.
Prevention
Prevention of obstructive jaundice includes the following areas:
- timely detection and active treatment of gallstone disease, chronic infections of the hepatobiliary system;
- proper nutrition (restriction of fried, fatty and rich in extractives food, adherence to the diet);
- refusal to abuse alcoholic beverages;
- maintaining an active lifestyle;
- normalization of body weight.
Possible complications
With the timely initiation of therapy, the prognosis is favorable. It worsens when the bile duct is compressed by a malignant tumor. If the patient does not receive timely surgical treatment, serious complications develop:
- cirrhosis of the liver;
- bilirubin encephalopathy;
- sepsis;
- acute (with complete blockage of the bile duct) or chronic (with partial obstruction) hepatic failure.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!