- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Gastroenteritis in children
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms of gastroenteritis in children
- Diagnostics
- Treatment of gastroenteritis in children
- Potential consequences and complications
- Forecast
- Prevention
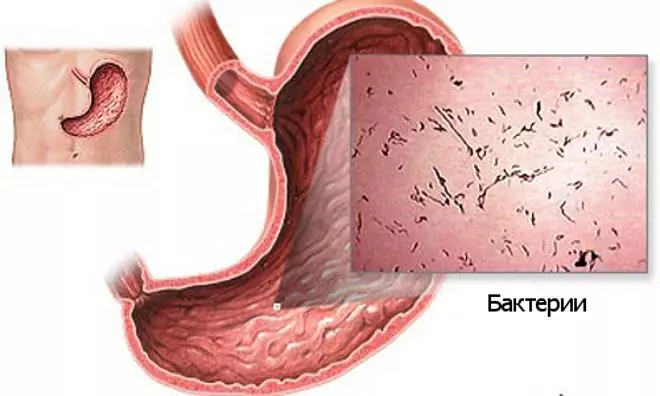
Gastroenteritis in children is an inflammatory lesion of the mucous membrane of the stomach and small intestine, manifested by nausea, vomiting, abdominal pain, and frequent loose stools. The occurrence of gastroenteritis in children may be associated with the action of various factors, but in pediatric practice, an infectious form of the disease is most often observed, which is most characteristic of children of early and preschool age.
The pathology is widespread, in the general structure of morbidity it ranks second, second only to influenza and respiratory viral infections. In developing countries, it is the leading cause of infant mortality. Gastroenteritis in children can be both an independent disease and a syndrome that forms against the background of acute infectious intestinal infections (salmonellosis, cholera).

Gastroenteritis - an inflammatory lesion of the mucous membrane of the stomach and small intestine
Causes and risk factors
The development of gastroenteritis in children can be caused by exposure to infectious and non-infectious agents that irritate the mucous membrane of the digestive tract and disrupt their functions. These include:
- viruses (intestinal adenoviruses, caliciviruses, rotaviruses, coronaviruses, astroviruses);
- bacteria (Escherichia coli, Salmonella, Shigella, Campylobacter);
- protozoa (cryptosporidia, dysentery amoeba, intestinal lamblia);
- helminths (crooked heads);
- food allergens (crabs, strawberries, chicken eggs);
- poisonous mushrooms (false mushrooms, fly agaric);
- toxic fish products (mackerel caviar, burbot liver);
- some medicines (iodine and bromine preparations, sulfonamides, antibiotics, non-steroidal anti-inflammatory drugs).

Gastroenteritis in children is most commonly associated with infectious agents
Provoking factors:
- plentiful coarse food rich in fiber;
- hot spices;
- cold carbonated drinks;
- general hypothermia;
- intestinal dysbiosis;
- hypovitaminosis conditions.
Bacteria, viruses, poisonous substances or allergens entering the gastrointestinal tract damage the epithelial cells of the mucous membrane, thereby causing an inflammatory process. The biologically active substances formed during this irritate the nerve endings, which causes abdominal pain, nausea, and vomiting. In addition, inflammation damages the villi of the small intestine. This disrupts the process of digestion, absorption of water, electrolytes and nutrients, leading to an increase in osmotic pressure in the lumen of the small intestine. As a result, diarrhea (frequent loose stools) occurs.
Viruses and bacteria in the process of vital activity synthesize toxins that are absorbed into the bloodstream and spread throughout the body, causing signs of general intoxication (fever, headache, lack of appetite), characteristic of acute gastroenteritis in children of infectious genesis.
Forms of the disease
Depending on the duration of the course, gastroenteritis in children is divided into acute and chronic forms. Acute gastroenteritis is characterized by severe clinical symptoms and lasts 7-10 days. The chronic form of the disease is characterized by a cyclical course, in which remissions are replaced by periods of exacerbation.
Depending on the etiological factor, the following forms of acute gastroenteritis in children are distinguished:
- viral - the causative agents are viruses, the mechanism of transmission is fecal-oral. Outbreaks of the disease are mainly observed during the cold season. The incubation period is 1-3 days. Symptoms of gastroenteritis in children in this case are often combined with ARVI symptoms (sore throat, dry cough, runny nose);
- bacterial - caused by pathogenic bacteria. The incubation period is short, usually less than 24 hours. Epidemiological outbreaks are more often recorded in summer. The disease proceeds with pronounced signs of general intoxication and lesions of the gastrointestinal tract;
- toxic - provoked by the ingestion of various toxic substances (salts of heavy metals, household chemicals, poisonous mushrooms, alcohol and many others);
- helminthic - associated with parasitizing worms, which in the process of life damage the mucous membrane of the small intestine. Symptoms of gastroenteritis in children with this form are usually erased, resembling a chronic form of pathology. The disease is recorded throughout the year;
- allergic (eosinophilic) - develops with hypersensitivity to certain foods that act as allergens. Most often these are eggs, cereals, dairy products. An allergic reaction is accompanied by the migration of eosinophils into the intestinal and gastric mucosa, which leads to its inflammation, the formation of infiltrates and dysfunction;
- alimentary - provoked by errors in nutrition, eating food that is inappropriate for age. Lasts 1-2 days.
According to the peculiarities of the clinical course of acute gastroenteritis in children, three degrees of severity of the disease are distinguished:
- Lightweight. Body temperature is not elevated, vomiting is absent or single, diarrhea no more than 3-5 times a day, signs of dehydration are absent.
- Average. The body temperature rises to 38-39 ° C, the child complains of pain in the abdomen. Repeated vomiting occurs, and the frequency of bowel movements can reach 10 times per day. The loss of electrolytes and water with feces and vomit leads to the development of a mild degree of dehydration, which is manifested by a loss of up to 3% of body weight, tachycardia, decreased urine output, dry mouth and increased thirst.
- Heavy. Body temperature reaches 40-41 ° C, repeated vomiting with an admixture of bile, stool frequency 15-20 times per day. Severe dehydration develops - body weight loss exceeds 4%, dryness of the mucous membranes and skin, impaired consciousness, cyanosis, a significant decrease in the number of urinations and the amount of urine discharge, convulsions are noted.
Symptoms of gastroenteritis in children
The clinical picture of chronic and acute gastroenteritis in children varies significantly depending on the form. Acute gastroenteritis occurs suddenly and develops rapidly. Its main symptoms are nausea, vomiting, abdominal pain and diarrhea. If the disease is caused by infectious agents, then the child's body temperature rises, a headache appears, and appetite decreases.

Acute gastroenteritis develops violently, with nausea, vomiting, severe abdominal pain, diarrhea
With vomit and feces, water and electrolytes are lost, which leads to dehydration of the body. The child is very thirsty, the amount of urine he has decreases, its color becomes saturated and dark.
Exacerbations of chronic gastroenteritis in children are provoked by an error in diet, stress, ARVI. Most often they occur in spring and autumn. During an exacerbation, the child develops abdominal pain, nausea, flatulence, rumbling, polyfecal matter (an abnormally large amount of feces), or diarrhea.
With a long course of the inflammatory process, a gradual damage to the villi of the small intestine occurs. As a result, nutrient absorption deteriorates and a number of general symptoms develop:
- weight loss;
- trophic changes in the skin, hair, nails;
- weakness;
- increased fatigue;
- irritability;
- sleep disorders.
In chronic gastroenteritis in children, general symptoms persist in the remission phase of the disease.
Diagnostics
Diagnosis of acute gastroenteritis in children is carried out on the basis of the characteristic clinical picture of the disease and the results of laboratory tests:
- general blood analysis;
- hematocrit;
- serological studies;
- coprogram;
- general urine analysis;
- bacteriological examination of feces with an antibioticogram.
If chronic gastroenteritis is suspected, not only laboratory, but also instrumental diagnostic methods are used:
- FEGDS;
- Ultrasound of the abdominal organs;
- intragastric pH-metry.

Abdominal ultrasound helps confirm the diagnosis of gastroenteritis in children
Treatment of gastroenteritis in children
Treatment of acute gastroenteritis in children begins with the appointment of a water-tea break for a period of 8-12 hours. At this time, the child is not fed, often give him a drink of warm liquid (unsweetened tea, solution of Regidron or Peditrala, mineral water without gas) 1-2 sips every 5-10 minutes. If indicated, gastric lavage is performed and a cleansing enema is given. After the end of the water-tea break, the child is assigned a medical nutrition (diet No. 4 according to Pevzner), the main purpose of which is mechanical, thermal and chemical sparing of the digestive system.
With a severe form of gastroenteritis in children, treatment is carried out in a hospital, since in this case dehydration develops rapidly and it may be necessary to intravenously infuse electrolyte and glucose solutions.

With gastroenteritis in children, diet No. 4 according to Pevzner is prescribed
For bacterial gastroenteritis, antibiotics are prescribed.
In case of a disease of allergic etiology, it is necessary to exclude a product that is an allergen from the diet. This is usually enough to quickly improve the child's condition.
With chronic gastroenteritis, you must follow a diet. Drug treatment is carried out taking into account the etiology. So, if a child has an increased acidity of the stomach, proton pump inhibitors, antacids are prescribed, and if inflammation of the mucous membrane of the stomach and intestines is caused by an infection, antibacterial therapy is indicated.
Potential consequences and complications
Acute gastroenteritis in children can lead to the development of serious complications:
- violation of water and electrolyte balance;
- hypovolemic shock;
- infectious toxic shock;
- acute renal failure;
- multiple organ failure.
Acute gastroenteritis is especially dangerous in children in the first years of life, as they quickly develop dehydration, a severe form of which can be fatal.
Forecast
With timely treatment started, the prognosis is generally favorable. In most cases, acute gastroenteritis in children ends with recovery within 7-10 days.
In chronic gastroenteritis, proper nutrition and anti-relapse courses of therapy (in autumn and spring) allow you to achieve a stable remission.
Prevention
Prevention of gastroenteritis in children includes:
- thorough hand washing;
- compliance with the technology of cooking and storage of dishes;
- using only tap or bottled water for drinking and cooking;
- isolation of patients with infectious forms of gastroenteritis and disinfection measures in the focus of infection.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!