- Author Rachel Wainwright [email protected].
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Nonspecific ulcerative colitis

Ulcerative colitis is a disease that has a chronic course and is characterized by ulcerative-inflammatory lesions of the mucous membrane of the large intestine.
The disease most commonly affects people between the ages of 20 and 40. It almost never occurs in people over 40 or under 15. The likelihood of ulcerative colitis is 15% higher if close relatives have this bowel disease.
Causes of occurrence
The exact causes of ulcerative colitis have not yet been established. It is assumed that its development is influenced by genetic, immunological, infectious factors, as well as various environmental factors. Most researchers suggest that the disease is autoimmune or genetically determined. Emotional factors play a significant role in the occurrence of exacerbations of ulcerative colitis, but in themselves do not lead to the development of this disease.
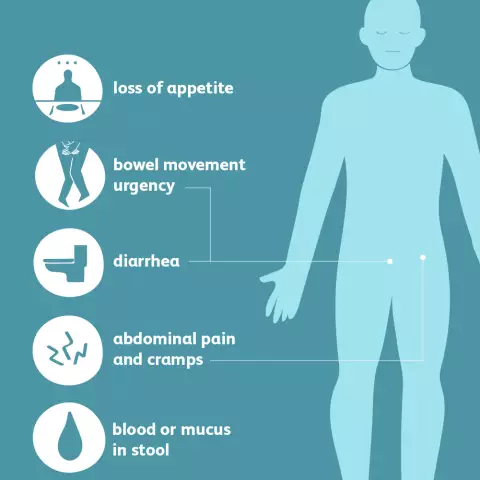
Ulcerative colitis: symptoms
The disease can start acutely or develop gradually. All symptoms of ulcerative colitis are caused by a chronic ulcerative inflammatory process in the mucous membrane of the large intestine. These include:
- Mushy stools or diarrhea mixed with mucus, pus and blood in the stool. Often, patients have false and rather painful urge to defecate - tenesmus;
- Pain in the left side of the abdomen. Sometimes they spread throughout the abdomen;
- Increased body temperature;
- Weight loss;
- Lack of appetite;
- Varying severity of water and electrolyte imbalance.
Extraintestinal symptoms of ulcerative colitis include:
- Arthritis and spondylitis;
- Blepharitis, conjunctivitis, iritis;
- Stomatitis;
- Cholelithiasis, cholangitis, cirrhosis;
- Nephrolithiasis;
- Erythema, pyoderma gangrenous;
- Thromboembolism and thrombophlebitis.
Complications
Like any other disease, ulcerative colitis can lead to the development of various complications:
- Toxic megacolon. With it, a significant expansion of the lumen of the transverse colon occurs. This complication occurs in 5% of cases and is often fatal;
- Perforation of ulcers of the large intestine. It is observed in 3 - 4% of patients and in 70 - 100% of cases leads to their death;
- Colon or rectal strictures - narrowing of the intestinal lumen in a certain area, which disrupts the passage of feces and can cause intestinal obstruction;
- Intestinal bleeding. This complication occurs in 6% of cases;
- Acute toxic dilation (expansion) of the colon. It is relatively rare;
- Perianal complications, which include cracks, fistulas, paraproctitis. These complications are observed in 30% of patients;
- Colon cancer. Patients who have been suffering from ulcerative colitis for more than 10 years have an increased risk of developing colon malignant neoplasms. Moreover, each year of the existence of this disease increases this risk by 2%.
Diagnostics
The diagnosis of ulcerative colitis is based on the characteristic clinical symptoms of the disease, medical examination data, laboratory diagnostics (fecal culture, scatological and histological analyzes) and instrumental diagnostics (X-ray and endoscopic examinations).
Ulcerative colitis: treatment
All patients with a newly diagnosed disease or with the development of an exacerbation must be hospitalized. Conservative treatment of ulcerative colitis includes the following components:
- Infusion therapy - is carried out to correct violations of water and electrolyte balance and detoxification;
- Vitamin therapy;
- Antibiotic therapy (prescribed after bacteriological examination of feces);
- Sedatives;
- Antidiarrheal therapy;
- Sulfasalazine;
- Cytostatics;
- Corticosteroid hormones.
It is very important to follow a diet high in digestible proteins in case of ulcerative colitis.
Surgical treatment of ulcerative colitis is carried out with the development of complications of the disease (massive bleeding, intestinal perforation, cancer, intestinal obstruction, etc.).
Ulcerative colitis: diet
During the period of exacerbation of the disease, it is necessary to adhere to the most gentle diet. After acute manifestations, such as abdominal pain, diarrhea, have subsided, the patient can be transferred to a less strict diet, in which it is allowed to include not pureed dishes.
It is very important that all dishes are not only tasty, but also varied. Patients are recommended steamed or boiled lean meat, mashed porridge, eggs, dry biscuits, dried white bread, rosehip broth, some juices (tomato, orange), compotes from ripe berries and fruits. Walnuts must be included in the diet for ulcerative colitis. But fried, salty, fatty or spicy dishes, legumes, chocolate, raw vegetables and fruits, mushrooms, beets, dried apricots, kiwi, plums should be completely excluded.
The diet for ulcerative colitis involves eating food in small portions over relatively short periods of time (fractional meals). This is due to the fact that a large amount of food will not be fully digested and assimilated, and in addition, it can provoke an increase in diarrhea.
Ulcerative colitis: alternative treatment
In many cases, doctors recommend to their patients not only medication, but also alternative treatment of ulcerative colitis. Microclysters with sea buckthorn or rosehip oil are quite effective in the treatment of this disease. In addition, you can use a decoction of the medicinal burnet inside. It is taken one tablespoon five times a day before meals. The course of treatment is at least a month.
However, alternative treatment of ulcerative colitis should in no case completely replace traditional drug therapy. This is a very serious chronic disease that can lead to the development of deadly complications, and its treatment must necessarily be carried out only under the guidance of a doctor!
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!