- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Shoulder arthrosis
The content of the article:
- Causes and risk factors
- Forms
- Stages
- Symptoms of arthrosis of the shoulder joint
- Diagnostics
- Treatment of arthrosis of the shoulder joint
- Possible complications and consequences
- Forecast
- Prevention
Arthrosis of the shoulder joint is a chronic disease caused by progressive degenerative-dystrophic changes in cartilage and bone tissue. At the final stage of the pathological process, there is a characteristic deformation of the joint and persistent dysfunction of the limb.

Signs of arthrosis of the shoulder joint
Causes and risk factors
The root cause of arthrosis of the shoulder joint is the lack of synovial fluid, which provides lubrication of the rubbing surfaces of the articular heads. It is not known for certain at what moment the pathological mechanism is triggered. Most likely, we are talking about a cumulative effect with the simultaneous action of a number of damaging factors. On the other hand, the structural features of the shoulder joint mitigate the manifestations of degenerative processes: this is one of the most mobile joints in humans, experiencing less support loads compared to the knee or hip joint.
As in the case of other degenerative-destructive pathologies, the main risk factor for the development of arthrosis of the shoulder joint is age over 45 years. According to the WHO, early signs of the disease are present in 10% of the population at the age of 55, while in the age group of 65 years and older, the incidence reaches 70%.
Overweight, injuries to the articular structures, in particular dislocations and injuries of the rotator cuff, unsuccessful attempts at reduction, as well as prolonged disproportionate loads on the shoulder increase the likelihood of early manifestation of the disease. The risk group includes professional athletes and persons engaged in hard manual labor - miners, builders, plasterers, painters, loaders, etc.

Predisposing factors for the development of arthrosis of the shoulder joint are injuries, especially dislocations
Decompensated metabolic disorders play a significant role in the pathogenesis of arthrosis. The deposition of crystals of calcium salts in the articular cavity and insufficient nutrition of the cartilage tissue can lead to disease over time. In some cases, arthrosis of the shoulder joint is a complication of acute and chronic arthritis.
Hereditary predisposition and birth defects of the shoulder joint also contribute to the development of pathology. At the same time, the tolerance of the articular structures to physical exertion and the ability of the cartilaginous tissue to restore are reduced.
Forms
In orthopedic practice, a distinction is made between primary and secondary arthrosis of the shoulder joint. In the first case, we are talking about the natural wear and tear of the cartilage as a result of aging; in the second case, the influence of provoking factors is clearly traced.
Secondary post-traumatic arthrosis of the shoulder joint in young people, caused by a one-time extreme load, strong blow or compression, is usually classified as a separate category due to the specificity of therapeutic measures. It is important to start treatment as early as possible, while the cartilage is still capable of regeneration, to avoid scarring and replacement of the cartilage with fibrous tissue.
Stages
Arthrosis of the shoulder joint is prone to a progressive course. Depending on the degree of damage, three stages of the pathological process are distinguished.
- There are aching pains in the shoulder, aggravated at night, in inclement weather and with high-amplitude movements of the hand, especially during abduction. Joint mobility is not impaired.
- The pain is permanent and spreads from the shoulder to the scapula. Against the background of prolonged muscle spasm, stiffness of movements appears in the shoulder joint, abduction of the limb is accompanied by a crunch and severe pain; joining hands behind the back is difficult.
- The final stage of the disease is characterized by severe pain in the shoulder region, pronounced deformation and almost complete immobilization of the joint: lifting and abduction of the limb is impossible, the ability to swing the hand forward and backward remains.
The third stage of arthrosis of the shoulder joint is relatively rare; in most patients, the pathological process stops at one of the two previous stages. Rapidly progressive degenerative-dystrophic changes in the shoulder joint are more often observed in patients who continue to load the shoulder joint, despite the obvious signs of the disease.
Symptoms of arthrosis of the shoulder joint
Moderate discomfort in the shoulder area is often attributed to a long stay in an uncomfortable position, however, the pulling nature of the pain, a painful reaction when pressing on the scapula and the lower part of the clavicle, periodic exacerbations after physical exertion and in cold damp weather give reason to suspect the initial stage of arthrosis. The painful sensations themselves are not always concentrated in the joint.
Sometimes pain spreads to the entire shoulder area, radiating to the back muscles from the side of the affected joint or to the elbow. In some cases, the disease manifests itself only as sharp pain after intense exercise, and at rest, the joint does not cause concern to the patient. With arthrosis of the shoulder, degenerative-dystrophic processes often involve the subacromial joint - the junction of the humerus and the acromial process of the scapula.

A sign of arthrosis of the shoulder joint is a pulling pain in the shoulder, pain when pressing on the scapula and the lower part of the clavicle
When examining a patient, the doctor pays attention to the size and shape of the shoulder joint, crunching and grinding with hand movements, the presence of erythema, crepitus and edema. In the later stages of the disease, the position of the limb is usually forced; bony protrusions are clearly visible at the junction of the scapula with the humerus.
The characteristic symptoms of arthrosis of the shoulder joint are found mainly during radiography, MRI and CT. The initial stage of the disease is characterized by the annular shape of the articular cavity - the so-called. ring symptom. At the second stage, characteristic changes in the articular structures are seen on X-ray images of the shoulder: narrowing of the joint space, subchondral edema, sclerotic foci, thickening of the joint capsule and bone heads, the appearance of osteophytes.
Diagnostics
A presumptive diagnosis is made by an orthopedist or rheumatologist based on physical examination data, taking into account the patient's history and complaints; functional tests with shoulder stress are also performed. In order to visualize specific changes in the cartilaginous and adjacent bone tissue, an X-ray of the shoulder in the axial and anteroposterior position is prescribed. In the early stages of the disease, MRI and CT are required for reasons of better visualization of minor changes in cartilage tissue. To identify the inflammatory process, it is necessary to pass a general and biochemical blood test and a general urine test.

X-ray helps to confirm the diagnosis of arthrosis of the shoulder joint
Treatment of arthrosis of the shoulder joint
The choice of a therapeutic strategy depends on the stage and severity of the disease, the nature of functional limitations and the individual characteristics of the organism. In the early stages, course conservative treatment is effective, aimed at the following tasks:
- anesthesia;
- restoration of joint mobility;
- slowing down degenerative processes in cartilage tissue.
To reduce joint pain, external, oral and injection analgesics are used. When a concomitant inflammatory process is detected, non-steroidal anti-inflammatory drugs are included in the drug regimen, among which the most common are cyclooxygenase-1 (COX-1) inhibitors. Intra-articular administration of corticosteroids is practiced only in the most severe cases when other drugs have failed.
Eating foods containing collagen also helps to maintain joint performance. Sources of natural collagen include poultry, in particular turkey, red fish and seafood - shrimp, mussels, crabs. It is recommended to limit the use of salt and hot spices, and also include in the diet foods rich in vitamins and minerals: fresh vegetables and fruits, herbs, sea onions and kelp.

Collagen-containing foods are beneficial for arthrosis of the shoulder
After the relief of acute pain, courses of hardware physiotherapy and massage, physical therapy and swimming are shown. Hilt therapy, cryotherapy, ultrasound and shock wave therapy have proven themselves well.
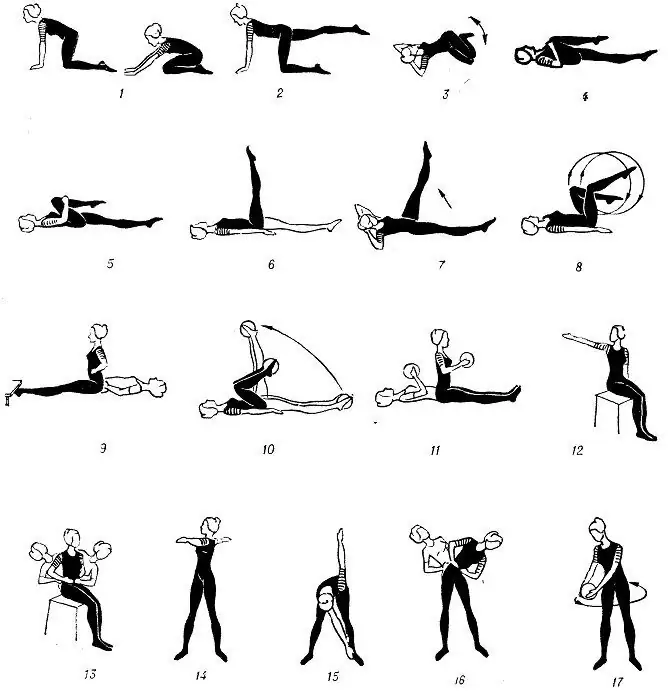
Therapeutic exercises for arthrosis of the shoulder joint can be performed at home and takes no more than half an hour a day. The technique of performing the exercises is not difficult, the main thing is to avoid sudden movements and not to miss classes. The most famous exercises for arthrosis of the shoulder joint include:
- swaying the hand at the elbow back and forth while sitting;
- lifting and lowering the shoulder girdle;
- girth of the shoulders from a position with arms crossed on the chest;
- shoulder rotation;
- turning the shoulders back with hands clasped behind.
In the first days, it is recommended to repeat each exercise no more than 5-8 times, gradually increasing the number of repetitions up to 10-15 times.
In severe cases that are not amenable to conservative treatment, the question of surgical intervention arises. A wide range of surgical methods for treating arthrosis of the shoulder joint has been developed:
- capsular release - removal of altered areas of the articular capsule to relieve the articular surfaces and restore passive joint mobility;
- synovectomy - removal of inflamed areas of the synovium, shown when it is impossible to stop the inflammatory process by conservative methods;
- debridgement is an arthroscopic surgical treatment that involves the removal of unstable areas of cartilage, chondromic bodies and other mechanical irritants. Debridging is most justified for patients under 60 years of age with moderate pain syndrome with significant limitation of joint mobility;
- endoprosthetics - replacement of the epiphysis of the humerus and subacromial joint with prostheses. In the future, endoprostheses will have to be replaced every 10-15 years.

Shoulder arthroplasty is indicated in the late stage of the disease
Indications for endoprosthetics in the late stages of arthrosis are intractable joint pain, foci of necrosis in the cartilage tissue, irreversible damage to the rotator cuff, and unsuccessful attempts to achieve improvement through minimally invasive surgical procedures.
It is not recommended to install an endoprosthesis in case of neuropathic joint syndrome, shoulder instability, paralysis of the deltoid muscle and rotator cuff muscles, acute or recent infection. If there are contraindications to endoprosthetics in patients under the age of 45-60, arthrodesis can be considered as an alternative - fixation of the humerus head in order to reduce pain during movement of the limb.
Postoperative rehabilitation begins the day after surgery. Stretching should be done for the first 6-8 weeks for optimal flexibility and a gradual increase in range of motion, after which exercises can be included to strengthen the shoulder muscles. It can take up to two years for a limb to fully recover.
Possible complications and consequences
In the absence of adequate treatment, arthrosis of the shoulder joint can lead to complete immobilization of the limb. With prolonged use of COX-1 inhibitors, side effects from the gastrointestinal tract are often manifested, ranging from dyspeptic disorders to bleeding and peptic ulcer disease; cases of renal failure are also known.
Forecast
With adequate treatment of primary arthrosis, patients under 35 years of age have a chance to achieve a complete cure. In the case of secondary arthrosis, the prognosis is more cautious, since complete restoration of the cartilage is impossible. With a properly selected therapy regimen and strict adherence to the doctor's recommendations, it is possible to slow down the development of the pathological process and prevent the transition of the disease to the terminal stage and the formation of disability.
Prevention
Prevention of arthrosis of the shoulder joint involves timely treatment of injuries, balanced nutrition, rejection of bad habits and an active lifestyle without excessive physical exertion. In the post-traumatic period and in old age, it is recommended to eat foods rich in collagen. To prevent exacerbations, it is recommended to avoid hypothermia, not to lift heavy loads and periodically undergo maintenance therapy.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!