- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Can pneumonia flow without temperature
The content of the article:
- Classification of pneumonia
- Etiology of pneumonia
- Pathogenesis of pneumonia
- The clinical picture of pneumonia
- Diagnostics
- Treatment
- Complications
- Video
Pneumonia without fever occurs only in rare cases. Usually this is due to the individual characteristics of the body or is noted against the background of violations of thermoregulation processes in both adults and children. Also, the asymptomatic course of the pathology can be observed in elderly and senile patients.

Pneumonia without fever is rare
But most often the disease is accompanied by a pronounced febrile reaction and intoxication, since a focus of acute inflammation is formed in the lungs, the cause of which is various bacterial and viral pathogens.
Pneumonia is an acute infectious and inflammatory disease characterized by focal lesions of the respiratory parts of the lungs and proceeds with severe fever, intoxication, clinical and radiological changes.
Regardless of whether the pathology is manifested by a pronounced increase in body temperature or not, it practically does not differ in etiology, pathogenesis and therapy. However, the latent form of the disease is considered more dangerous, leading to the generalization of inflammation with the development of serious complications, which in most cases is associated with a delayed diagnosis and a late start of treatment.
Classification of pneumonia
According to the etiological factor, pneumonia is divided into the following types:
- bacterial;
- viral;
- ornithosis;
- rickettsial;
- mycoplasma;
- fungal;
- mixed;
- allergic, or infectious-allergic;
- pneumonia of unknown etiology.
Due to the fact that timely verification of the causative agent of the disease is not always possible, a working classification of pneumonia has been adopted, which is based on the clinical and etiological principle, taking into account the epidemic situation and risk factors:
- community-acquired acquired pneumonia;
- nosocomial acquired (hospital, or nosocomial) pneumonia;
- pneumonia in immunodeficiency states;
- aspiration pneumonia.

Hospital pneumonia develops during the patient's stay in a medical facility for another disease
The most common form is community-acquired pneumonia. It has the most characteristic clinical picture and is caused mainly by bacteria. Most often, pathology occurs in closed groups (schoolchildren, students, military) and can have the character of an epidemic outbreak.
Hospital pneumonia is pneumonia that developed within 48-72 hours or more after an adult or child was admitted to the hospital for another illness. To the nosocomial form of the disease can lead to previous operations, artificial ventilation of the lungs, various endoscopic manipulations and previous treatment with broad-spectrum antibiotics.
Pneumonia, which develops against the background of an altered immune status, occurs in patients with AIDS (acquired immunodeficiency syndrome), patients with systemic diseases, and also against the background of immunosuppressive treatment.
Aspiration pneumonia can occur in people suffering from alcoholism and drug addiction, when inhaled into the lungs of various substances in a massive volume, such as vomit. Also, the disease can develop after anesthesia, with depression of consciousness and against the background of gastroesophageal reflux (reverse reflux of stomach contents into the esophagus).
Etiology of pneumonia
In community-acquired pneumonia up to 90% of cases, the causative agents are: pneumococcus (Streptococcus pneumoniae), Haemophilus influenzae, Mycoplasma pneumoniae and Moraxella catarrhalis (Moraxella catarrhalis) - the pathogen, which is a gram-negative microflora of the coccus respiratory tract. Less often, chlamydia or Klebsiella (Friedlander's stick) leads to the development of the disease.

In 90% of cases of community-acquired pneumonia, the causative agent of the disease is bacteria, in particular pneumococcus
The cause of nosocomial pneumonia can be enterobacteriaceae, Pseudomonas aeruginosa, Staphylococcus aureus and anaerobes. The same pathogens lead to the development of pathology in patients with an immunodeficiency state. Viruses and fungi are also an etiological factor.
Among the viruses, the causative agents of plague, typhoid fever, measles, rubella, cytomegalovirus can be the cause of the disease.
Anaerobic bacteria, gram-negative flora, Staphylococcus aureus act as an etiological infectious agent in aspiration pneumonia.
During an influenza epidemic, a combined infection with a viral-bacterial association of microorganisms is possible.
Pathogenesis of pneumonia
A pathogenic microorganism, entering the lungs along with the inhaled air, finds itself on the surface of the epithelial cells of the bronchial tree and damages the cell membrane, promoting the formation of biologically active substances - cytokines.
Cytokines are markers of inflammation. Under their influence, the migration of macrophages, neutrophils and other cells involved in the local inflammatory reaction to the focus of damage occurs.
After the invasion of the pathogen, the production of endo- and exotoxins, inflammation of the alveoli and bronchioles with the development of clinical signs of the disease occurs.
Thus, taking into account the etiology and pathogenesis of the disease, it can be concluded that pneumonia without temperature is practically impossible. And a pronounced increase in body temperature is a sign of inflammation - a protective and adaptive reaction of the body in response to the introduction of a foreign agent and tissue damage.
The clinical picture of pneumonia
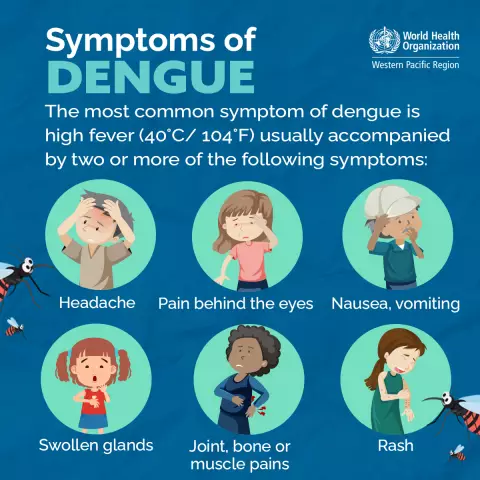
The symptoms of the disease are combined into several syndromes:
- general intoxication syndrome: includes general weakness, weakness, headaches, pain in muscles and joints, shortness of breath, tachycardia, loss of appetite, pallor of the skin and visible mucous membranes;
- syndrome of general inflammatory changes: includes symptoms such as fever up to febrile numbers (above 38.0 ° C), chills;
- syndrome of inflammatory changes in the lung tissue: the patient has a cough, sputum leaves, the frequency and nature of respiratory movements change, up to the onset of respiratory failure;
- syndrome of involvement of other organs and systems: a systemic inflammatory reaction or spread of infection can lead to pathology of the cardiovascular system, organs of the gastrointestinal tract, kidneys and nervous system.
Symptoms may vary from patient to patient.
Symptoms of the disease can be different in people of different constitutions, ages, depending on the state of reactivity of the body, the presence of concomitant diseases of other organs and systems.
The severity of violations characterizes the severity of the pathology - mild, moderate or severe.
Diagnostics
When making a diagnosis, the doctor relies on the patient's complaints, clinical manifestations of the disease, the results of tests and X-ray studies.
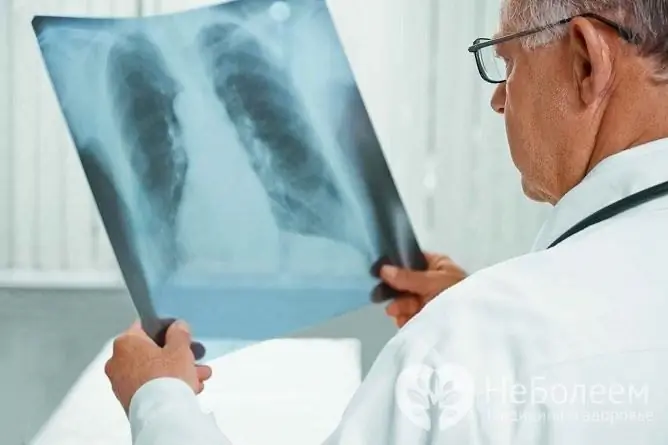
To make a diagnosis, you should consult a doctor and conduct the necessary research
When examining the patient, there is a shortening of the percussion sound, an increase in voice tremor, the appearance of wet wheezing. The affected side of the chest lags behind when breathing.
X-ray examination allows you to identify a lesion in the corresponding segment or lobe of the lung, to detect effusion in the pleural cavity.
In the blood test, changes in acute phase blood parameters are noted: leukocytosis with a leukocyte shift to the left, an increase in ESR (erythrocyte sedimentation rate), an increase in the concentration of fibrinogen, alpha2-globulins and the appearance of C-reactive protein.
Before the appointment of antibacterial treatment, a bacteriological examination of sputum or bronchial lavages is carried out, which makes it possible to detect the pathogen and determine its sensitivity to antibiotics.
Additionally carried out:
- electrocardiography (ECG): allows you to assess the state of the myocardium;
- spirometry: it is necessary to assess the function of external respiration and the state of bronchial patency.
In some cases, bronchoscopy and computed tomography are recommended to clarify the diagnosis.
Treatment
Patients with pneumonia are subject to hospitalization, but it is possible to organize a hospital at home, provided that full care is provided and all the prescriptions of the attending physician are observed.

With an uncomplicated course of pneumonia, treatment can be carried out at home
Bed rest, plenty of drink, food rich in vitamins and proteins are recommended.
An important role in the treatment of pneumonia belongs to antibacterial drugs, which eliminate the cause that led to the development of the disease. They have a bactericidal and bacteriostatic effect.
Preference is given to broad-spectrum antibiotics, which are prescribed for up to 10-14 days. The drugs of choice are: Amoxiclav, Ceftriaxone, Azithromycin, Levofloxacin.
Pathogenetic and symptomatic treatment is aimed at improving pulmonary ventilation and blood circulation, increasing the body's immunoreactive capacity, restoring impaired bronchial patency. Anti-inflammatory, desensitizing and antipyretic drugs are prescribed.
Thanks to expectorant, then antitussive drugs, the patient coughs with sputum production against the background of anti-inflammatory and antibacterial treatment.
Complications
If the pathology is not diagnosed or treated in a timely manner, pulmonary and extrapulmonary complications may develop. This situation is especially common in cases of atypical onset and course of the disease, including pneumonia without fever.
Major complications:
- abscess formation;
- pleurisy or pleural empyema;
- attachment of the asthmatic component;
- acute respiratory failure;
- infectious toxic shock;
- myocarditis;
- endocarditis;
- meningitis;
- hepatitis;
- glomerulonephritis;
- sepsis.
Video
We offer for viewing a video on the topic of the article.

Alina Ervasova Obstetrician-gynecologist, consultant About the author
Education: First Moscow State Medical University. THEM. Sechenov.
Work experience: 4 years of work in private practice.
Found a mistake in the text? Select it and press Ctrl + Enter.