- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Cough in a child at 2 years old: how to treat at home
The content of the article:
- Cough in a 2-year-old child: treatment with medications
- Inhalation
- Folk remedies
- Distracting procedures
- What is a cough and what causes it
- Video
Cough in children is quite common. Naturally, its appearance, especially in babies of the first years of life, causes concern for parents. In this article, we will look at how to treat a cough in children at 2 years old.

There can be many reasons for the development of cough attacks in a 2-year-old child, before giving medications, it is required to find out the cause
Cough in a 2-year-old child: treatment with medications
Cough is a symptom of many and sometimes very serious diseases. And therefore, his treatment should be carried out only as prescribed by a doctor. The wrong choice of antitussive drugs can seriously harm a child's body.
The following drugs are used to treat cough:
| Group name | Mechanism of action |
| Centrally acting antitussives with narcotic effect (Codeine, Dexometorphan, Morphine) | They inhibit the activity of the cough center of the brain. Application in young children is possible only in a hospital setting |
| Centrally acting antitussives without narcotic effect (Tusuprex, Sinekold, Libeksin, Glaucina hydrochloride) | Suppress the activity of the cough center. Do not cause respiratory depression and addiction. Prescribed only for dry, painful cough, such as whooping cough |
| Coating agents (various syrups and lozenges containing wild cherry, licorice, acacia, eucalyptus, honey, glycerin extracts) | They form a protective layer on the mucous membrane of the oropharynx. They are prescribed to reduce irritation of the mucous membrane of the upper respiratory tract. |
| Expectorants (Licorice root syrup, Althea root syrup) | They reduce the viscosity of bronchial secretions and increase their volume, which improves the expectoration of sputum. In children in the first years of life, use with caution, as vomiting associated with cough may increase |
| Mucolytics (Ambroxol, Lazolvan, Bromhexin) | Liquefies phlegm, thereby improving its coughing. Bromhexine can increase bronchospasm, therefore it is not prescribed during an attack of bronchial asthma |
| Antihistamines (Zodak, Tavegil, Suprastin) |
Appointed only for allergic cough. Have a drying effect on the mucous membrane of the respiratory tract, which can further intensify dry cough |
| Bronchodilators (Euphyllin, Theophylline, Atropine) | Shown for bronchospasm. Atropine is rarely used in pediatric practice, as it increases the viscosity of sputum |
Antitussive medicines for children are best used in the form of syrups or drops. These "baby" dosage forms provide accurate dosing. In addition, they taste good, and a 2-year-old child takes them with pleasure.
Inhalation
One of the most effective remedies is aerosol inhalation, which can be carried out at home using a nebulizer. Aerosol (small particles of liquid and drugs) moisturizes the mucous membrane of the respiratory tract, reduces irritation, and dilutes phlegm.
For inhalation, you can use:
- physiological sodium chloride solution;
- sodium bicarbonate solution;
- degassed alkaline mineral waters;
- medications.
For inhalation in children of two years old, no more than 1.5 ml of solution should be used. You can repeat the procedures no more than 2-3 times a day.
Folk remedies
In the treatment of children in the first years of life, methods of traditional medicine can also be used. They are not effective enough to replace the main treatment if necessary, but they can be used as an adjunct to it if such an addition is required and agreed with the attending physician.
As expectorants, for example, decoctions of the following medicinal plants are used:
- thermopsis;
- thyme;
- violets;
- pine buds;
- licorice;
- plantain;
- mother and stepmother;
- ipecacuanas;
- oregano;
- elecampane;
- anise;
- marshmallow.
The mechanism of action of these medicinal plants includes the following links:
- liquefaction of bronchial mucus;
- increased secretory activity of the bronchial glands;
- improvement of the motor function of the ciliated epithelium and muscles of the bronchioles;
- activation of the respiratory center.
Parents should be aware that the natural origin of medicines is not a guarantee of their safety for the baby's body. Alternative methods of treatment have a number of contraindications, and in addition, their use may be accompanied by the development of side effects.
Plants such as ipecacuanha and thermopsis have an irritating effect on the gastric mucosa, due to which reflex stimulation of the vomiting center of the brain occurs. In this regard, they should not be used in children with diseases of the central nervous system. Side effects of these plants can be:
- vomiting;
- the formation of atelectasis;
- aspiration of vomit;
- asphyxia.
Oregano, licorice and anise have not only expectorant, but also a pronounced laxative effect. Therefore, they are not prescribed for children with diseases of the gastrointestinal tract, accompanied by diarrhea.
Decoctions of expectorant medicinal herbs begin to have a therapeutic effect quickly only if they are taken often, every 3-4 hours. This causes a negative reaction in the sick baby, provokes crying, which, in turn, increases the cough.
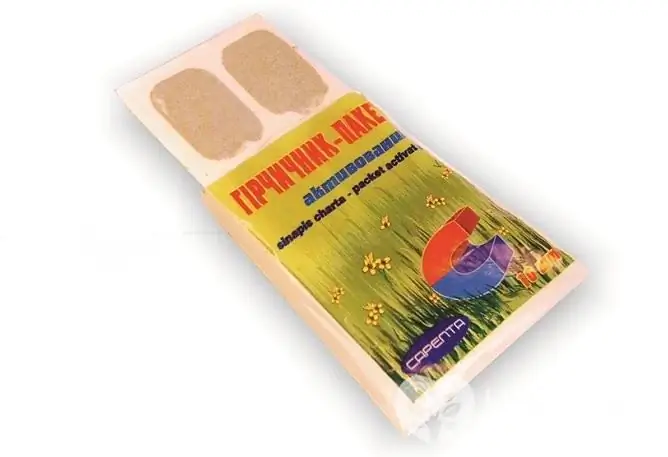
Mustard plasters are contraindicated for young children
Distracting procedures
Many adults remember how, in childhood, with colds, mothers and grandmothers put them cans or mustard plasters. Currently, the attitude of doctors towards these procedures has changed. We will try to explain why.
Previously, the therapeutic effect of cans and mustard plasters was associated with an improvement in blood flow to the diseased organ. But the reddened skin under the mustard plaster or the formation of a hematoma at the place where the jar was placed does not at all indicate that the processes of increasing blood circulation began in deeper tissues, including the bronchi and lungs.
The reflexogenic effect of mustard plasters and cans is also questionable, since it is impossible to prove it. These procedures are quite painful and are always accompanied by the baby's discomfort and crying. Against the background of crying, the depth and frequency of breathing increases, which, in turn, activates the blood flow in the lungs.
What is a cough and what causes it
A cough is a complex reflex act that restores normal airway patency. It can be dry and wet (wet). In the latter case, the child coughs up phlegm.
The reasons for its occurrence can be:
- infectious and inflammatory processes of the upper (pharyngitis, tonsillitis, sinusitis, laryngitis) and lower (tracheitis, bronchitis, pneumonia) parts of the respiratory system;
- bronchospasm (obstructive bronchitis, allergic cough, bronchial asthma);
- airway obstruction with viscous sputum, foreign bodies;
- irritation of the pleura (pleurisy);
- heart failure;
- stomach diseases.
The intensity of cough in children is different, ranging from rare coughs to severe attacks to vomiting. In the first case, the child usually does not need antitussive therapy, but it should still be shown to the doctor and the necessary examination should be carried out in order to identify the underlying disease.
Video
We offer for viewing a video on the topic of the article.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
Found a mistake in the text? Select it and press Ctrl + Enter.






