- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Leishmaniasis
Brief description of the disease

Leishmaniasis is an infectious disease caused by the simplest parasites - Leishmanias. Small blood-sucking insects, mainly mosquitoes and mosquitoes, act as carriers of infection. In urban settings, leishmaniasis spreads through sick people and dogs. The disease has spread in Uzbekistan, Transcaucasia, Turkmenistan, in some countries of Asia and Africa. Outbreaks of infection occur between May and October, when the causative agent is most active. The risk group includes persons newly arrived in the endemic focus. Permanent residents of problem regions develop cutaneous leishmaniasis much less frequently.
Types of leishmaniasis
Experts distinguish two main forms of the disease: cutaneous leishmaniasis and internal (visceral) leishmaniasis.
Visceral leishmaniasis begins gradually. The incubation period lasts from 10-20 days to several months. In the early stages, leishmaniasis manifests itself as minor bowel disorders and an increase in weakness. Typical signs of leishmaneosis include enlargement of the spleen, lymph nodes, and liver. It comes to the point that at the height of the disease the spleen reaches a huge size and, due to the increase in weight, sinks into the small pelvis. Also, in patients, there is a change in the color of the skin (becomes pale, earthy) and the appearance of various kinds of rashes, for the most part pustular. In some cases, visceral leishmaniasis can cause swelling, anemia, bleeding, and weight loss.
An accurate diagnosis is made after puncture of the bone marrow and spleen for the presence of leishmania.
Urban cutaneous leishmaniasis
The symptoms of cutaneous leishmaniasis appear after 3 to 8 months. In the place where the parasites have invaded the body, a small tubercle with a diameter of 1-4 mm appears. As leishmaniasis develops, it grows in size and becomes covered with a scaly crust. Removal of the tubercle is fraught with the formation of a bleeding ulcer, covered with a purulent plaque, and an infiltrate, the disintegration of which causes the expansion of the skin lesion zone. There are from 1 to 10 such ulcers on the human body. As a rule, they are located on the face and hands, that is, in those places that are accessible to mosquitoes.
Rural cutaneous leishmaniasis
This form has a shorter incubation period. A cone-shaped tubercle appears at the site of penetration of pathogens. It grows rapidly in size and often reaches 1-2 cm in diameter. In the center of the tubercle, tissue necrosis occurs, which, after rejection, form an ulcer. If there are few ulcers, then they are quite extensive, reaching 6 cm in diameter. A large number of small ulcers (tens and hundreds of formations) restrains the increase in individual affected areas. When cutaneous leishmaniasis is diagnosed, symptoms persist for several months, after which the ulcers clear up.
Note also that both urban and rural cutaneous leishmaniasis can develop into a chronic form, which resembles lupus in a number of ways.
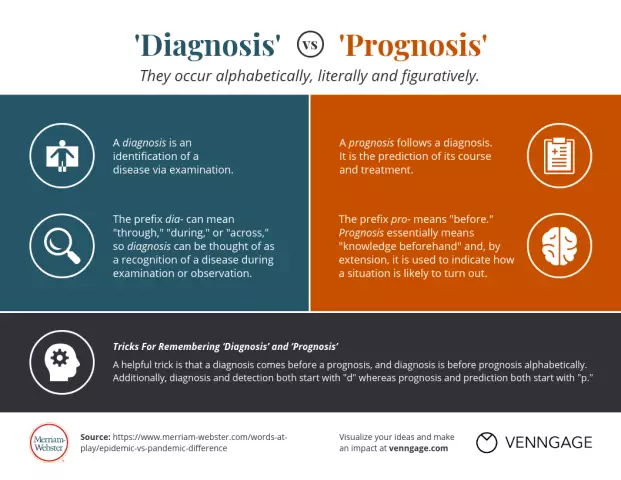
Diagnosis of the disease
All forms of leishmaniasis must be distinguished from sarcoidosis, leprosy, tubercular syphilis, and tuberculous lupus. Differential diagnosis is carried out on the basis of anamnestic data and information about the patient's stay in endemic foci. Experts get the final data on the presence of infection after examining the tests that determine the presence of Leishmania in the body.
As for the specific differences between the infection in question from other diseases. While tuberculous lupus erythematosus predominantly affects children, leishmaniasis, which often requires treatment for adults, does not depend on the patient's age. In addition, the bumps on the skin with leishmaniasis are much denser, which means there is no effect of the probe falling through. It is also worth noting that the rashes are not prone to ulceration, although they are located on the scars. The latter are deeper and more elongated, while in lupus, scars are most often superficial.

Cutaneous leishmaniasis differs from tubercle syphilis in the location of the rash. As a rule, it is located in open areas of the body, has a lower density of tubercles, ulcerates later and does not give a positive serological reaction to syphilis. There are also differences in the nature of the scars. With leishmaniasis, they are more retracted, and with tubercle syphilis, they are mosaic.
Leishmaniasis - treatment and prevention
Patients are prescribed monomycin. It is injected intramuscularly 3 times a day. The standard dosage is 250,000 units. The course of treatment lasts 10-12 days until the time when cutaneous leishmaniasis disappears completely. When symptoms worsen, it is recommended to use monomycin ointment.
Prevention of cutaneous leishmaniasis is based on the control of mosquitoes and mosquitoes, the destruction of stray dogs and rodents. In recent years, attempts have been made to prevent cutaneous and visceral leishmaniasis through the preventive administration of live cultures of the pathogen.
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!