- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Multiple myeloma
The content of the article:
- Causes and risk factors
-
Forms
X-ray forms
- Disease stages
- Myeloma symptoms
- Diagnosis of multiple myeloma
-
Myeloma treatment
- Antineoplastic treatment
- Supportive care
- Possible complications and consequences
- Forecast
- Prevention
- Video
Multiple myeloma is a type of blood cancer, a malignant transformation of plasma cells (differentiated B-lymphocytes, a subtype of leukocytes that are part of the immune system and synthesize antibodies that help the body fight infections). Normally, the bone marrow produces plasma cells (plasma cells) and B-lymphocytes in the amount required by the body. At some point, this process fails, and instead of normal cells, atypical (tumor) plasma cells begin to be produced, which gradually replace normal cells in the bone marrow. Instead of antibodies, these cells produce paraproteins, proteins that damage kidney tissue.

Myeloma is characterized by multiple lesions, primarily of flat bones, including the bones of the skull
Multiple tumor foci occur in myeloma, primarily in the bone marrow, but also in bones (often flat, such as cranial bones and ribs, but tubular bones, in particular, the femur, can also be damaged), lymph nodes and other organs. The multiplicity of lesions is due to another name for multiple myeloma - multiple myeloma. Since tumor cells produce paraprotein, which refers the disease to paraproteinemic hemoblastosis, malignant immunoproliferative diseases.
Basically, elderly people - 70 years and older are susceptible to myeloma, although young people under 40 years old also occasionally get sick, men are somewhat more likely than women (the ratio of sick men and women is 1.4: 1). For an unknown reason, this disease in people of the Negroid race occurs twice as often as in any other.
Synonyms: multiple myeloma (MM), plasmacytoma, Rustitsky-Kalera disease (named after the scientists who first described the disease).
Myeloma code according to ICD 10 - C90 (multiple myeloma and malignant plasma cell neoplasms).
Causes and risk factors
The reason for the malignancy of plasma cells has not been established. Presumably, there is a genetic predisposition. Viral infections, ionizing radiation (including radiation therapy), carcinogens, cytostatic drugs (chemotherapy), chronic intoxication can act as mutagenic factors. In 10% of people with monoclonal gammopathy, it transforms into myeloma.
Predisposing factors include everything that has a suppressive effect on the immune system: obesity, bad habits, an unhealthy lifestyle, stress instability, etc.
Forms
There are several classifications of MM.
By clinical manifestations:
- symptomatic;
- asymptomatic (smoldering);
- monoclonal gammopathy of undetermined significance (MGUS).
Cellular composition:
- flamocytic;
- plasmablastic;
- polymorphic cell;
- small cell.
Depending on the prevalence of foci:
- focal;
- diffuse focal;
- diffuse.
Depending on the type of paraprotein produced:
- G-myeloma (75% of all cases);
- A myeloma;
- D-myeloma;
- E-myeloma;
- Bence-Jones myeloma;
- M-myeloma;
- non-secreting (the last two are rare forms).
With the flow:
- slowly progressing;
- rapidly progressing.
X-ray forms
According to Reinberg:
- multiple focal;
- diffuse porotic;
- isolated.
According to Lemberg:
- focal;
- knotty;
- mesh;
- osteolytic;
- osteoporotic;
- mixed.
Disease stages
There are three stages in the course of multiple myeloma:
- Initial.
- Expanded.
- Terminal.
There are several criteria for determining them.
The International Scoring System (ISS) is focused on the amount of beta-2 microglobulin (β2M) and serum albumin:
- β2M <3.5 mg / L, albumin ≥ 3.5 g / dL.
- β2M <3.5 mg / l, albumin <3.5 g / dl; or β2M 3.5-5.5 mg / l, albumin does not matter.
- β2M ≥ 5.5 mg / l.
The ISS system has a number of limitations due to the fact that in some cases the levels of albumin and beta-2 microglobulin can change under the influence of concomitant diseases, for example, diabetes mellitus. Therefore, it is recommended to correlate this staging system with the Dury - Salmon clinical classification (B. Durie, S. Salmon), according to which the stages are defined as follows:
- Hemoglobin> 100 g / l; blood calcium is the norm; serum paraprotein <50 g / l for IgG or <30 for IgA; excretion of Bens-Jones protein (immunoglobulin light chains) in the urine <4 g / day; single plasmacytoma or osteoporosis, or the absence of both (to determine stage I, all of the above criteria must be met).
- Criteria not meeting either Stage I or Stage III.
- Hemoglobin 120 mg / l; serum paraprotein> 70 g / l for IgG, and> 50 g / l for IgA; urinary excretion of Bens-Jones protein> 12 g / day; three or more foci of osteolysis (to determine stage III, compliance with only one of the listed criteria is sufficient).
Each of the three stages of the Dury-Salmon classification is divided into substages A and B, depending on the serum creatinine content, which serves as an indicator of kidney function:
- Creatinine <2 g / dL (<177 μmol / L).
- Creatinine> 2 g / dL (> 177 μmol / L).
Myeloma symptoms
Before the first symptoms appear, the disease progresses asymptomatically for a long time (this period can be from 5 to 15 years). At this time, a high ROE, paraproteinemia, and in the analysis of urine, proteinuria can be detected in a blood test. But since the number of plasma cells in the bone marrow is not increased, the diagnosis cannot be made.
The advanced stage is characterized by the appearance and growth of symptoms, which is manifested by a number of syndromes, which in different patients have different degrees of severity.
| Syndrome | Description |
| Bone damage | Symptoms are associated with both focal tumor growth of plasma cells in the form of bone tumors, and with the fact that plasma cells synthesize substances that promote lysis, i.e. destruction of bone tissue. First of all, flat bones (bones of the pelvis, skull, shoulder blades, ribs, spine) suffer, less often - tubular bones (femur, humerus). As a result, there is intense pain in the bones, aggravated by pressure, during movement, pathological (not caused by trauma) bone fractures, bone deformities appear. |
| Damage to the hematopoietic system | Leukopenia, thrombocytopenia, plasma cells in peripheral blood, increased ROE, myelogram content of plasma cells> 15% (in some forms of MM the myelogram may not have abnormalities). |
| Protein pathology syndrome | It is caused by the overproduction of paraproteins (pathological immunoglobulins or Bens-Jones protein), which is accompanied by hyperproteinemia (manifested by thirst, dry skin and mucous membranes), proteinuria, the appearance of cold antibodies (manifested by cold allergy, acrocyanosis, trophic disorders in the limbs), amyloid those parts of the body where amyloid deposition has occurred, an increase in the lips and tongue). |
| Myeloma nephropathy | It is observed in 80% of patients with MM, characterized by the development of chronic renal failure, which is manifested by weakness, nausea, decreased appetite, and weight loss. Edema, ascites, hypertension (one of the diagnostic signs) are not characteristic. |
| Visceral syndrome | As a result of tumor plasma cell infiltration, lesions of the liver, spleen (more often), gastrointestinal tract, pleura (less often) develop in all internal organs with the development of characteristic symptoms. |
| Secondary immunodeficiency | Susceptibility to infections, common respiratory viral diseases are severe, often complicated by the addition of a bacterial infection, infectious and inflammatory diseases of the urinary tract, shingles, fungal infections are not uncommon. |
| Increased blood viscosity | It is characterized by impaired microcirculation, which is manifested by visual impairment, muscle weakness, headache, the development of trophic skin lesions, thrombosis. It is observed in 10% of patients with MM. |
| Hemorrhagic syndrome | It develops due to a decrease in the functionality of platelets and the activity of blood coagulation factors. Manifested by bleeding gums, nosebleeds, multiple hematomas. |
| Neurological syndrome | It is caused by plasma cell infiltration of the dura mater, deformation of the bones of the skull and vertebrae, compression of the nerve trunks by tumors. It manifests itself as peripheral neuropathy, muscle weakness, deterioration of all types of sensitivity, paresthesias, decreased tendon reflexes and other symptoms depending on the area of the lesion. |
| Hypercalcemia | It is caused by the leaching of calcium from the bone tissue due to lysis. It is manifested by nausea, vomiting, drowsiness, disorders of consciousness, loss of orientation. |
The terminal stage is characterized by exacerbation of existing symptoms, rapid destruction of bones, proliferation of tumors into neighboring tissues, increasing renal failure, severe anemia, and infectious complications.
Diagnosis of multiple myeloma
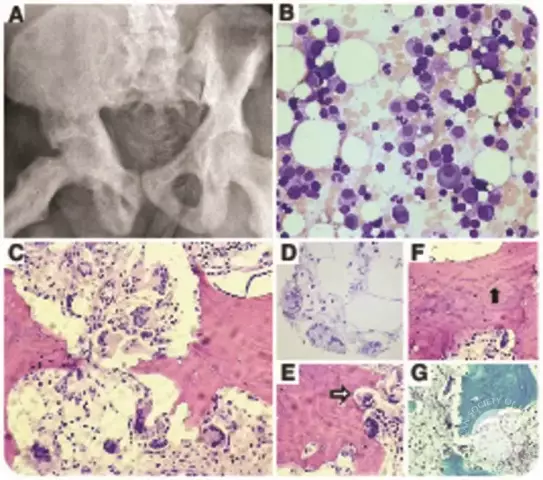
The main signs of multiple myeloma are bone marrow plasmacytosis (> 10%), foci of osteolysis, M-gradient (monoclonal protein) or Bence-Jones protein in serum or urine. It is on these signs that a diagnostic search is carried out with a suspicion of a disease, and for the diagnosis it is sufficient to establish plasmacytosis and the M-gradient (or Bens-Jones protein), regardless of the presence of bone changes.

With multiple myeloma, an excess amount of plasma cells is found in the bone marrow
The following diagnostic methods are used:
- X-ray of the skull, chest, pelvis, spine, shoulder girdle, humerus and femur.
- Spiral computed tomography.
- Magnetic resonance imaging.
- Positron emission tomography.
- Bone marrow aspiration biopsy to determine the myelogram.
- Laboratory analyzes of blood and urine.
- Cytogenetic research.
Bone and extraosseous lesions in multiple myeloma are abbreviated as CRAB:
- C - Calcium (calcium) - hypercalcemia, Ca content> 2.75;
- R - Renal (renal) - impaired renal function, serum creatinine> 2 mg / dL;
- A - Anaemia (anemia) - normocytic and normochromic, hemoglobin <100 g / l;
- В - Bone (bone) - foci of osteolysis, pathological fractures, osteopenia, etc.
Differential diagnosis is carried out with the following pathologies:
- other monoclonal gammopathies;
- polyclonal hypergammaglobulinemia;
- reactive polyclonal plasmacytosis;
- bone metastases.
Myeloma treatment
Multiple myeloma is incurable, however, adequate treatment allows you to achieve a stable remission and maintain it for a long time.
Therapy is carried out in two directions: antitumor (etiotropic) and supportive (symptomatic).
Antineoplastic treatment
It is prescribed taking into account the patient's age and the presence of concomitant diseases. Patients under 70 years old or over 70 years old without concomitant pathology are prescribed 4-6 cycles of polychemotherapy, after which hematopoietic cells are mobilized, followed by high-dose chemotherapy (myeloablation) followed by supportive autologous stem cell transplantation. In the future, after 3-4 months, the expediency of several more courses of polychemotherapy or another autotransplantation of stem cells is being considered.
Patients who have contraindications to such treatment (patients over 70 years of age with concomitant pathology) are prescribed polychemotherapy.
Supportive care
It is carried out in the following areas:
- treating renal dysfunction;
- suppression of osteolysis;
- elimination of hypercalcemia;
- treatment of high blood viscosity syndrome;
- treating anemia;
- relief of pain syndrome;
- antithrombotic therapy;
- prevention of infection.
In the asymptomatic form of multiple myeloma, treatment is not required; medical supervision is sufficient.
Possible complications and consequences
Multiple myeloma can transform into acute plasmablastic leukemia or lymphosarcoma.
Forecast
Depending on the form of myeloma and the sensitivity to the treatment, 5-year survival can be achieved in 40-80% of patients. The unfavorable prognostic factors include relapses; after each relapse, remission is more difficult to achieve. Death in most cases occurs from severe infectious complications.
Prevention
Prevention of multiple myeloma consists in avoiding contact with carcinogens and toxic substances and maintaining a healthy lifestyle.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!