- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Human papillomavirus in women
The content of the article:
- Causes and risk factors
- Forms of the disease
- Human papillomavirus symptoms in women
- Diagnostics
- Treatment of diseases caused by the human papillomavirus in women
- Possible complications and consequences
- Forecast
- Prevention
The human papillomavirus in women is a group of the papillomavirus family that includes 27 species and more than 170 types, or strains.
Human papillomavirus
Human papillomavirus is highly contagious and widespread. According to various sources, from 60 to 90% of all persons of reproductive age are infected with the human papillomavirus. The largest number of cases of virus carriage is registered in the age group of 18-30 years. HPV is capable of provoking the development of benign and malignant neoplasms:
- HPV types 1-5, 7-10, 12, 14, 15, 17, 19-24, 26-29, 49, 57 are responsible for the appearance of warts (HPV 1, 2, 4 provokes plantar warts, HPV 10, 14, 15, 27, 28, 49 - flat, HPV 7 - Butcher's warts, HPV 2, 4, 27, 29, 57 - vulgar, HPV 3, 5, 8, 9 - filiform);
- HPV types 6, 11, 16, 18, 31, 33, 35, 42-44, 54 cause the formation of genital warts or papillomas of the genitals or respiratory tract;
- HPV types 16, 18, 30, 31, 33, 39, 40, 42, 43, 51, 52, 55, 57, 58, 59, 61, 62, 64, 67-70 can cause precancerous pathology, of which the highest strains 16 and 18 are oncogenic.
The human papillomavirus is transmitted from an infected person to a healthy person, while simultaneous or sequential infection with several types of the virus is possible.
Causes and risk factors
HPV enters the woman's body mainly through sexual contact (the probability of infection through sexual contact reaches 66%), but contact and household transmission is also possible. When it gets on the skin or mucous membranes, the virus enters a cell, inside which it can be in the cytoplasm (episomal, or benign form) or penetrate the cell nucleus and insert its genes into its genome (introsomal, or malignant form).
Risk factors for human papillomavirus infection in women include:
- infectious diseases of the genitourinary tract;
- early onset of sexual activity with frequent partner changes;
- unprotected sex;
- multiple abortions;
- immunodeficiency states;
- period of pregnancy;
- non-compliance with the rules of personal hygiene;
- bad habits.
The possibility of transmission of HPV during labor has not been fully determined. There is information about the detection of an infectious agent in children, as well as in girls before sexual activity. According to some reports, the DNA of the human papillomavirus is found in the aspirate from the nasopharynx of newborns in about 33% of cases.

The chance of contracting HPV through sexual intercourse is 66%
The risk of infection in women increases with hormonal disorders, frequent stress, hypothermia, and prolonged use of oral contraceptives.
Forms of the disease
The human papillomavirus is divided into three groups:
- non-oncogenic;
- low oncogenicity;
- high oncogenicity.
Depending on the characteristics of the clinical picture of the disease caused by HPV, the following forms of viral infection are determined:
- latent, or virus carrier - the virus does not manifest itself for a long time, it is usually detected during the diagnosis for another reason;
- subclinical - the virus causes the formation of neoplasms (condylomas and warts), which may not be visible to the naked eye due to their small size;
- clinical - the virus actively multiplies in the human body, leading to the formation of neoplasms visible to the naked eye.
When a virus affects the skin with the formation of warts, their following forms are: vulgar (simple, ordinary) warts, flat (youthful), plantar, filiform (papillomas, acrochords). HPV also causes the development of genital warts (anogenital papillomas).
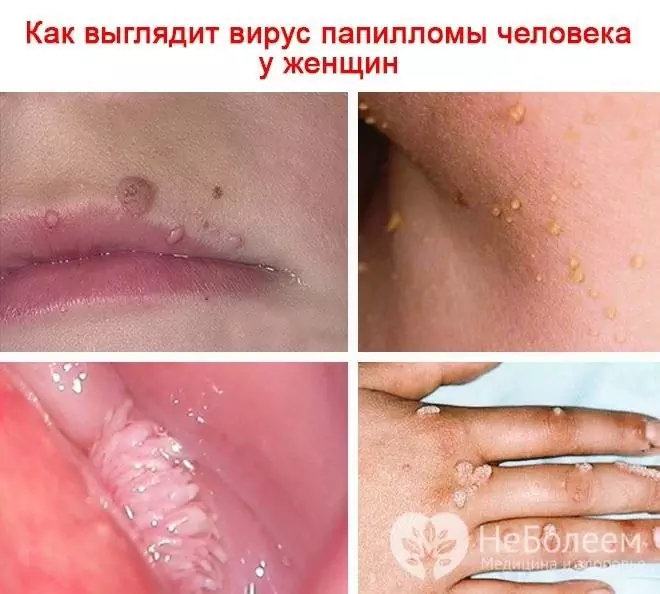
If the human papillomavirus in a woman infects the skin, warts, condylomas, papillomas appear
Respiratory recurrent papillomatosis, another disease caused by HPV, is classified as follows:
- youthful - the debut of the disease in infancy or at 11-12 years;
- adult - onset of the disease at 30-40 or after 60 years.
Human papillomavirus symptoms in women
The human papillomavirus in women in 13-34% of cases proceeds subclinically, a clinically pronounced pathological process is recorded in 1-3% of patients, in the rest the infection has a latent course. The infectious process in the genital area can be exacerbated against the background of vulvovaginitis, endocervicitis, as well as sexually transmitted diseases (chlamydia, genital herpes, gonorrhea, trichomoniasis, syphilis).
The most common symptoms of the human papillomavirus in women from the genitourinary system are itching and burning in the genital area, pathological vaginal discharge, pain during and / or after intercourse, dysuric phenomena. A specific sign of HPV lesions in the urogenital tract in women is condylomatosis of the vulva, vagina, and cervix. In persons who practice anogenital intercourse, papillomas are often located in the perineum and in the perianal region.

Itching and burning in the genital area is a common symptom of human papillomavirus in women
Depending on the type of virus that caused the development of the pathological process on the skin, the clinical manifestations of the disease may vary. Pathological changes in the skin, as a rule, are found 1-6 months after infection. The color of the skin on the affected areas usually does not change; in some cases, papillomas are white to brown. Papillomas are benign neoplasms of the skin and mucous membranes and are connective tissue growths protruding above the surrounding tissues. Since they contain blood vessels, they bleed when injured.
Vulgar warts have the appearance of a solid neoplasm with a diameter of more than 1 mm and a rough keratinized surface, prone to fusion with each other and damage to significant areas of the skin. In most cases, neoplasms are localized on the skin of the hands, usually located in groups, but in some cases there is a long existence of a single pathology. If the patient has chronic diseases, as well as in other immunodeficient conditions, the pathological process is prone to spread. In isolated cases, malignant degeneration of vulgar warts can occur.
With the development of plantar warts, a seal with a shiny surface and a protruding rim appears on the skin of the foot. In some cases, other smaller neoplasms appear around one wart. Warts on the foot are easily injured, after which they become painful, especially when walking. For the same reason, a secondary (bacterial) infection is added to them more often than to other neoplasms caused by HPV.

Plantar warts are caused by HPV
Flat warts appear as smooth, flat, rounded neoplasms that can have a pink or yellowish tint. Their difference from other warts in the absence of a layer of keratinization on the surface, as well as in the fact that they never form in the groin, on the skin of the palms and feet, and practically do not occur after 40 years.
Filiform warts, or papillomas, are diagnosed in about half of patients over 50 years old who have applied to a medical institution for skin neoplasms, and in the age group 80 years and older they are found in 100%. Usually, papillomas are localized around the eyes, on the neck, in the armpits, under the breast and in the groin. At first, they are small nodules that are not prone to keratinization and do not differ in color from the rest of the skin. In the future, the nodules increase in size, they have a thin leg. Papillomas are easily injured, while becoming inflamed and painful. Unlike most other warts, they are not prone to spontaneous self-resolution.
With the development of recurrent respiratory papillomatosis in patients, there is a proliferation of papillomas on the mucous membranes of the respiratory tract from the nasal cavity to the peripheral parts of the lungs, most often the mucous membranes of the larynx are affected. This pathology is manifested by hoarseness, weak cry. In severe cases (usually with concomitant immunodeficiency), airway obstruction.
Diagnostics
The complex of diagnostic measures for suspected HPV in women depends on the type of lesion and the localization of the pathological process. So, to identify filamentous warts, an examination is sufficient, and for some others, a complex analysis of the human papillomavirus in women by DNA diagnostics methods is required.
If the urogenital tract is affected by the human papillomavirus, a gynecological examination is carried out for the diagnosis, as well as:
- colposcopy (examination of the entrance to the vagina, the walls of the vagina and the vaginal area of the cervix using a colposcope);
- cytological examination of smears taken from the cervical canal and cervix;
- research by the method of polymerase chain reaction, which makes it possible to identify the presence and type of HPV.

If a woman is suspected of being infected with HPV, a colposcopy is recommended to assess the condition of the cervix
Neoplasms on the skin in some cases require identification using dermatoscopy, examination of scraping from the affected area by means of polymerase chain reaction.
Treatment of diseases caused by the human papillomavirus in women
Etiotropic treatment of human papillomavirus has not been developed, if necessary, symptomatic therapy is used. Neoplasms caused by the human papillomavirus must be removed.
Removal of papillomas, genital warts and warts is carried out by several methods, the most popular is electro-destruction. With the help of electro-destruction, it is possible to remove both single neoplasms and affect extensive affected areas. The negative aspects of electro destruction include the need for anesthesia, as well as the risk of scarring, especially with a large area of influence.

Papillomas, condylomas, warts caused by HPV in a woman are successfully removed with a laser
The method of cryodestruction, that is, destruction of tissues using ultra-low temperatures, allows you to remove neoplasms without anesthesia and without subsequent scar formation, but has limited application (it is inconvenient to use in hard-to-reach areas).
Laser therapy allows you to remove neoplasms without subsequent scarring and without injuring the surrounding tissues. This method requires local anesthesia.
If a possible malignancy is suspected, the neoplasm is removed with a scalpel with the capture of unaffected surrounding tissues, and then sent for histological examination.
If the virus affects the mucous membrane of the cervix, surgical treatment, laser or cryotherapy may be required.
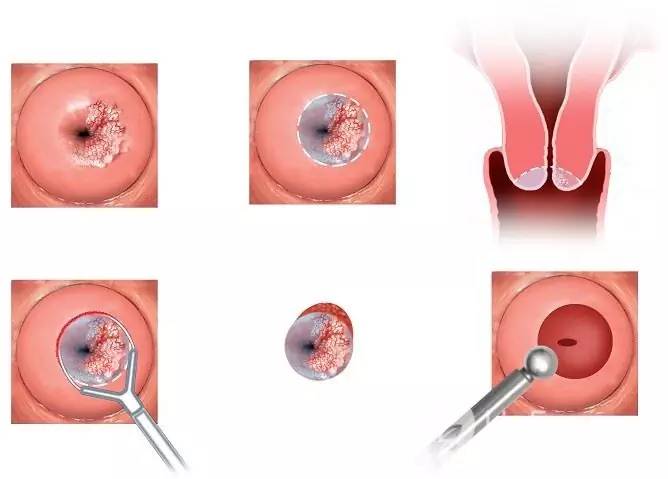
Conization of the cervix - a type of surgical treatment for damage to the cervix with human papillomavirus
The risk of relapse is high (about 30%) with any treatment method, since only the neoplasm caused by the virus is removed, and the virus itself remains in the body. In the case of generalized pathology, systemic antiviral therapy, the use of immunomodulators, and vitamin preparations may be appropriate.
Women who are planning a pregnancy and pregnant women with suspected infection with the human papillomavirus of the genital tract are recommended to be monitored by a gynecologist. Since antiviral therapy can have an adverse effect on the developing fetus, and the risk of transmitting the virus to the fetus is relatively low, treatment of the human papillomavirus in women during pregnancy is postponed until the birth of the child.
Possible complications and consequences
Neoplasms that occur when infected with the human papillomavirus in women are, in some cases, prone to malignant degeneration. Some types of papillomavirus contribute to the development of carcinoma of the nasopharynx, cervix, vulva and vagina, perianal malignant neoplasms.
Forecast
In some cases, self-resolution of neoplasms of the skin and / or mucous membranes caused by HPV infection is possible. With the development of warts on the skin in persons with normal immunity, as a rule, their spontaneous resolution is observed in about 67% of cases.
The prognosis is generally good. The exception is infection with oncogenic types of human papillomavirus.
Prevention
The measures of primary prevention of infection with oncogenic HPV strains include vaccination in women, which is most effective before sexual intercourse, and therefore is recommended at the age of 11-13, but can be carried out later (contraindicated during pregnancy and lactation).
In addition, in order to prevent infection of women with HPV, it is recommended to adhere to general preventive measures:
- compliance with the rules of personal hygiene;
- timely treatment of sexually transmitted infections;
- the use of barrier methods of contraception;
- refusal of casual sex;
- rejection of bad habits;
- strengthening the body's defenses (proper nutrition, good rest, sufficient physical activity, stay in the fresh air, etc.);
- avoiding hypothermia;
- avoidance of stress and mental strain.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!






