- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Amebiasis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms of amebiasis
- Diagnostics of the amebiasis
- Treatment of amoebiasis
- Potential consequences and complications
- Forecast
- Prevention
Amoebiasis is a protozoal anthroponous disease characterized by the development of ulcerative colitis and abscess formation of internal organs. It is widespread in countries with subtropical and tropical climates. In recent years, amoebiasis has begun to be diagnosed in other regions, which is explained by the development of foreign tourism and the growth of population migration, but epidemiological outbreaks are practically not observed here, the disease is recorded in the form of sporadic cases.
Amoebiasis most often affects older children and middle-aged people. In the overall structure of mortality from parasitic infections, it ranks second, second only to malaria.
Disease immunity is non-sterile. Immunity to infection persists only for the period of residence in the intestinal lumen of the pathogen of amoebiasis.

Entamoeba histolytica - the causative agent of amebiasis
Causes and risk factors
The causative agent of amoebiasis is Entamoeba histolytica (histolytic amoeba), which belongs to the simplest. The life cycle of the parasite is represented by two stages replacing each other depending on environmental conditions: cysts (dormant stage) and trophosite (vegetative form). The trozophyte goes through a number of developmental stages, in each of which it can stay for a long time:
- tissue form - characteristic of acute amebiasis, found in the affected organs, occasionally in the feces;
- large vegetative form - lives in the intestines, absorbs erythrocytes, is found in feces;
- luminal form - characteristic of chronic amoebiasis, is also found in remission in feces after taking a laxative;
- the precystic form, as well as the luminal form, is characteristic of chronic amebiasis and amebiasis in the stage of remission (convalescence).

Life cycle of Entamoeba histolityca in the human body
The source of infection are patients with a chronic form of amebiasis in remission and cyst carriers. In the acute form of the disease or exacerbation of the chronic, patients release into the environment unstable vegetative forms of Entamoeba histolytica, which do not pose an epidemiological hazard.
The mechanism of infection is fecal-oral. The route of transmission of the causative agent of amoebiasis is food, water, contact. Once in the lower gastrointestinal tract, mature cysts turn into a luminal, non-pathogenic form that feeds on intestinal bacteria and detritus. In the future, this form either turns into cysts again, or becomes a large vegetative form of the parasite. The latter secretes proteolytic enzymes that allow it to penetrate into the thickness of the intestinal wall, where it turns into a tissue form.
The tissue form of the causative agent of amebiasis parasitizes in the submucosa and mucous layer of the colon walls, leading to the gradual destruction of epithelial cells, the formation of microabscesses and microcirculation disorders. All this as a result becomes the cause of the formation of multiple ulcers of the large intestine. The pathological process is localized mainly in the region of the cecum and the ascending part of the colon, much less often affects the rectum and sigmoid colon.
With the blood flow, histolytic amoebas are carried throughout the body and enter the internal organs (pancreas, kidneys, brain, lungs, liver), leading to the formation of abscesses in them.
Factors that increase the risk of contracting amoebiasis are:
- low socio-economic status;
- living in regions with hot climates;
- non-compliance with the rules of personal hygiene;
- unbalanced diet;
- stress;
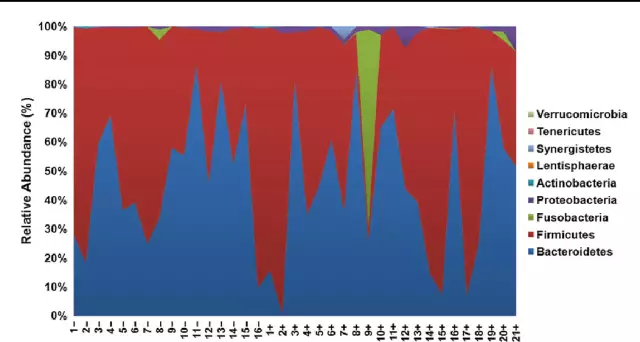
- intestinal dysbiosis;
- immunodeficiency.
Forms of the disease
On the recommendation of WHO, adopted in 1970, the following forms of amebiasis are distinguished:
- intestinal;
- extraintestinal;
- cutaneous.
Russian infectious disease specialists regard the cutaneous and extraintestinal form of the disease as a complication of the intestinal form.
Intestinal amebiasis can occur in the form of acute or chronic (recurrent or continuous) processes of varying severity.
Often amoebiasis is recorded as a mixed infection, simultaneously with other protozoal and bacterial intestinal infections.
Symptoms of amebiasis
The incubation period lasts from a week to several months, but most often it is 3-6 weeks.
Symptoms of amebiasis are determined by the clinical form of the disease.
With intestinal amebiasis, the patient develops and gradually increases pain in the abdomen. Frequent bowel movements occur. The feces contain significant amounts of mucus and blood, resulting in the characteristic appearance of raspberry jelly.
Simultaneously with the onset of symptoms of colitis, intoxication syndrome develops, which is characterized by:
- subfebrile fever (less often it can be febrile in nature, that is, over 38 ° C);
- general weakness, decreased performance;
- arterial hypotension;
- tachycardia;
- decreased appetite.
The acute course of the intestinal form of amebiasis without treatment lasts 4-6 weeks. Spontaneous recovery and complete sanitation of the patient's body from the pathogen is extremely rare. Most often, without treatment, the disease turns into a chronic recurrent form, in which exacerbations occur every few weeks or months.

Multiple ulcers with intestinal amebiasis
The chronic form of intestinal amebiasis without adequate therapy lasts for decades. It is characterized by the development of disorders of all types of metabolism (anemia, endocrinopathy, hypovitaminosis, exhaustion up to cachexia). When chronic amebiasis is combined with other intestinal infections (salmonellosis, shigellosis), a typical clinical picture of a severe intestinal disease is formed, accompanied by pronounced signs of intoxication and serious disturbances in the water-electrolyte balance.
The extraintestinal manifestation of amebiasis is most often amoebic liver abscess. Such abscesses are multiple or single abscesses localized in the right lobe of the liver, devoid of the pyogenic membrane.
The disease begins with a sudden rise in temperature to 39-40 ° C, which is accompanied by severe chills. The patient has severe pains in the right hypochondrium, which are aggravated by changing the position of the body, sneezing, coughing. The general condition is rapidly deteriorating. The liver increases significantly in size and becomes sharply painful on palpation. The skin acquires an earthy color, in some cases jaundice develops.
Amoebic pneumonia occurs with pronounced inflammatory changes in the lung tissue. The disease has a long course and, in the absence of specific therapy, can lead to the formation of lung abscesses.
Amebic meningoencephalitis (amoebic abscess of the brain) occurs with pronounced symptoms of intoxication and the appearance of cerebral and focal neurological symptoms. For amoebic meningoencephalitis, the formation of multiple abscesses is characteristic, mainly localized in the left hemisphere.
Attention! Photo of shocking content.
Click on the link to view.
The main symptom of cutaneous amoebiasis is a slightly painful ulcer with an undermined uneven edges, which have an unpleasant odor. Most often, ulcers form on the skin of the perineum, genitals, as well as in the area of postoperative wounds and fistulas.
Diagnostics of the amebiasis
Diagnosis of amebiasis is carried out on the basis of characteristic clinical symptoms, data from an epidemiological history, as well as the results of laboratory and instrumental studies.
The diagnosis is confirmed by the detection of large vegetative and tissue forms of the causative agent of amebiasis in feces, sputum, abscess contents, separated from the bottom of ulcerative defects. For the purpose of their detection, microscopy of native smears, stained according to Heiderhain or Lugol's solution, is performed. The detection of luminal, precision forms of Entamoeba histolytica or cysts in a smear indicates only the infection of the subject, and not the presence of a disease.
In the laboratory diagnosis of amebiasis, the following methods are used:
- cultivation of amoebas on artificial nutrient media;
- contamination of laboratory animals;
- serological research (ELISA, RIF, RNGA).
If necessary, perform colonoscopy or sigmoidoscopy, computed tomography, and general X-ray of the abdominal cavity.

The diagnosis of "amebiasis" is based on the results of laboratory tests
In the general analysis of blood, changes are revealed that are characteristic of any acute inflammatory process (leukocytosis, a shift in the leukocyte formula to the left, an increase in the erythrocyte sedimentation rate).
Amoebiasis requires differential diagnosis with the following diseases:
- acute intestinal infections with signs of colitis (balantidiasis, salmonellosis, escherichiosis, shigellosis);
- non-infectious colitis (ischemic colitis, Crohn's disease, ulcerative colitis);
- purulent cholecystocholangitis;
- malignant neoplasms of the large intestine;
- hepatocellular carcinoma;
- echinococcosis of the liver;
- malaria;
- right-sided exudative pleurisy;
- dermatomycosis;
- tuberculosis;
- skin cancer.
Treatment of amoebiasis
Hospitalization with amebiasis is indicated only in the case of a severe course of the disease or the development of its extraintestinal forms. In other cases, the treatment of amebiasis is carried out in a polyclinic setting.
With asymptomatic carriage of histolytic amoeba, as well as for the prevention of exacerbations, luminal amoebicides of direct action are prescribed. In the treatment of intestinal amoebiasis, as well as amoebic abscesses, tissue amoebicides are used, which have a systemic effect. Specific treatment of amebiasis cannot be carried out during pregnancy, since these drugs have a teratogenic effect, that is, they can cause fetal abnormalities.

For asymptomatic amebiasis, oral amebicides are indicated
With the ineffectiveness of conservative therapy and the threat of the spread of a purulent process, indications for surgical intervention arise. With small single amoebic abscesses, it is possible to puncture them (performed under ultrasound control), followed by aspiration of purulent contents and rinsing the cavity with a solution of amoebicidal drugs. In case of large abscesses, surgical opening of their cavity is performed, followed by its drainage.
Severe necrosis of the intestinal wall around the amoebic ulcer or its perforation are indications for emergency surgical intervention - resection of the large intestine, in some cases, colostomy may be required.
Potential consequences and complications
Complications of the intestinal form of amebiasis are:
- perforation of the intestinal wall with the development of peritonitis - a complication characteristic of severe forms of the disease and is the cause of mortality in 20-45% of deaths from amebiasis. Clinically manifested by the emergence and rapid increase in the intensity of the severity of the acute abdomen symptom complex;
- penetration of ulcers of the large intestine into other organs of the abdominal cavity;
- pericolitis - is recorded in 10% of patients with amebiasis. It is characterized by the development of adherent fibrous peritonitis more often in the region of the cecum or the ascending part of the colon. The main clinical sign of the disease is the formation of a painful infiltrate with a diameter of 3-15 cm, an increase in body temperature, and local tension of the muscles of the anterior abdominal wall. Pericolitis responds well to specific treatment and does not require surgical intervention;
- amoebic appendicitis is an acute or chronic inflammation of the appendix. Surgical intervention in this case is undesirable, as it can provoke generalization of the invasion;
- intestinal obstruction - develops as a result of cicatricial strictures of the large intestine, characterized by a clinic of low dynamic intestinal obstruction with typical pain syndrome, palpable painful dense infiltration, bloating and asymmetry of the abdomen;
- amoebic tumor (amoeba) is a rare complication of amebiasis. Formed in the ascending or cecum, much less often in the splenic or hepatic flexures of the colon. It does not require surgical treatment, since it responds well to specific conservative therapy.
More rare complications of the intestinal form of amoebiasis are prolapse of the rectal mucosa, polyposis of the large intestine, intestinal bleeding.
The most dangerous complication of extraintestinal amebiasis is perforation of the amoebic abscess. Breakthrough of hepatic amoebic abscess can occur in the subphrenic region limited by adhesions, abdominal cavity, bile ducts, chest, subcutaneous or perirenal tissue. This complication is observed in 10-20% of cases of liver amebiasis and is accompanied by a very high mortality rate (50-60%).
Forecast
Without adequate treatment, amebiasis takes a protracted chronic course, is accompanied by the development of abscesses in the internal organs, a violation of all metabolic processes, and eventually becomes the cause of the patient's death.
Against the background of the specific therapy, the patients' health condition improves rapidly.
In some patients, after the end of the course of therapy for amebiasis, complaints of manifestations of irritable bowel syndrome persist for several weeks.
Recurrences of amebiasis are possible.
Prevention
To prevent further spread of infection, the following sanitary and epidemiological measures are carried out:
- the isolation of a patient with amoebiasis is stopped only after complete sanitation of the intestine from histolytic amoebas, which should be confirmed by the results of a six-fold study of feces;
- convalescents are monitored by an infectious disease specialist for 6-12 months;
- surrounded by the patient, regular current disinfection is carried out using a 2% cresol solution or a 3% lysol solution.
In order to prevent infection with amebiasis, you should:
- carefully observe personal prevention measures;
- wash vegetables and fruits under running tap water, pour boiling water over them;
- do not drink water from questionable sources (it is best to give preference to bottled water from well-known manufacturers).
Individuals traveling to epidemiologically unfavorable regions for amebiasis are prescribed individual chemoprophylaxis using universal amoebicidal agents.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!