- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Treatment of phobias and emotional addictions
Conceptualizing Dependencies
In the International Classification of Diseases (ICD-10), addiction syndrome is a combination of behavioral, cognitive and physiological manifestations that develop after repeated use of a psychoactive substance. Typically, we are talking about a strong desire to use the substance, a problem with self-control and control of use, which in the sick person has a higher priority than other actions. All this leads to harmful consequences: social, psychological and physical.

Source: depositphotos.com
Nine psychoactive substances are identified: alcohol, opioids, cannabinoids, sedatives and hypnotics, cocaine, psychostimulants, hallucinogens, nicotine and organic solvents. Each of these types of substances causes a specific type of addiction, has its own characteristics and predetermines the characteristics of treatment.
Clinical conditions that can occur include acute intoxication, use in which health damage occurs by the substance itself or the way it is used, addiction syndrome, withdrawal syndrome, psychotic disorder, and amnestic syndrome (memory disorder).
Predisposing factors
The modern understanding of the formation of addiction is based on the interaction of many factors: the specific action and effect of the drug; availability; the social status of the consumer; portability; peer pressure, etc. Each of the factors operates at different levels in the process of creating and maintaining dependence.
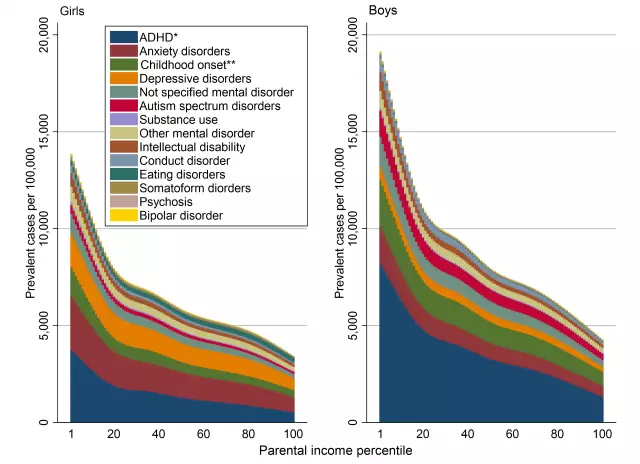
Thus, factors can be divided into: social and environmental; the reinforcing effect of the narcotic substance; learning and conditioning effect; the state of being canceled as a reinforcement; genetic predisposition; psychodynamic factors such as the role and function of the family and the structure of the consumer's personality. In the general vulnerability model, 31% of the variables can be attributed to genetic factors, 25% are influenced by family and 44% are factors other than family.
Genetic factors. Twin studies show that, for example, alcohol dependence has its own genetic component (four times the risk of alcohol addiction in children of alcoholics). Other addictions are also more likely to be genetically determined.
Neurochemical factors. Mechanisms of action in the central nervous system have been found for most addictive substances. As a rule, psychoactive substances replace natural biochemical processes. For example, substances like heroin turn off the centers of pain impulses, the person ceases to feel pain and is in a state of euphoria. But gradually the body adapts and begins to build up pain impulses, so as to neutralize the effect of the drug. As a result, if the drug is stopped, the person experiences terrible pain, and subsequent drug use no longer brings such pleasure as before, already performing the function of a pain reliever.
Additional factors. The dependence involves the personal characteristics of the individual (they also have their own neurochemical correlate in the form of a violation of the reward system, etc.), the social context, attitude towards drugs and their use, the availability and rules of drug use, their legalization, pressure from interested groups. In addition, the issue of the impact of stress, frustration, trauma and conflict in a general sense, physically ill and other mental disorders is considered.

Deepest beliefs
According to cognitive theory, addiction is an extremely complex process characterized by deep-seated and persistent, low-adaptive beliefs. They are formed in early childhood, through exposure to critical experience, and from the very beginning have nothing to do with the use of alcohol and drugs. The formation of basic schemes is influenced by the family, social and cultural environment. Negative experiences in the early stages of development create patterns that lead to the vulnerability of their owners, remain latent until they are activated by any event (contact with a drug substance).
Such patients may be characterized by any negative beliefs about themselves: "I am bad," "I do not deserve love," "I am weak," "I am disgusting," etc. It is important to note that a certain short-term orientation is formed in childhood, when an individual seeks immediate deliverance, but does not set goals for the future. These children do not develop the ability to endure and cope with stress and frustration, and social and interpersonal skills do not develop. As a rule, such children are dependent on their parents and only then become addicted to drugs. They are socially unadapted, they form a negative attitude towards the world around them. Subsequently, the drug becomes a way of escape from the "bad world".
Example. Karl's mother constantly protected and took care of him. His father often drank, did not pay enough attention to his son, treated him and his mother with contempt. In cases where the father was "rowdy", the mother protected the child. Already in an older age, she continued to solve all his problems. Karl did not develop an active position, and his father's attitude made him perceive himself in a negative light.
Traumatic (initiating) situation
As mentioned above, the main triggering event for addiction is the first use of the drug. On the one hand, the very decision to use or experiment is influenced by the person's basic beliefs, and on the other hand, the fact of use predetermines the development of dysfunctional thinking. The first experience is usually pleasant, so the person will try to repeat it. This will reinforce his expectations and some of his beliefs about the drug. Further use reinforces concepts that become automatic and the vicious circle closes.
Example. Karl started drinking alcohol when he graduated from high school. He started drinking sutra already and continued throughout the day.
Intermediate Beliefs
At the onset of addiction, drug use turns out to be a compensatory strategy that develops by creating new beliefs about the drug, which are then combined with pre-existing maladaptive beliefs. In addition, dysfunctional assumptions arise, such as "if … then …", which further weaken the person before using the drug ("If I drink, I will feel better; If I do not smoke a cigarette now, I will have a seizure"). In fact, the individual creates for himself "permissive" beliefs, with which he justifies the use of a narcotic substance.
Example. Over time, alcohol became Karl's primary way of dealing with problems. Carl enjoyed the alcoholic effects: he loved the feeling of relaxation, the taste of alcohol, and the social context after drinking with friends. From his point of view, there were no negative consequences, they were caused by other people, for example, the police or his wife. Thus, Karl developed a cognitive link "if I take alcohol, I will get rid of my problems." Alcohol for the patient has also become a means of interacting with other people: "Drinking is always fun in a group of people."
Current problem model
The biopsychosocial model of the disease (classical medical model) assumes that the dependent patient falls into several vicious circles.
A circle associated with biochemical changes. Initially, the primary use of the narcotic substance is positively reinforced, which leads to changes in the biochemistry of the central nervous system, and, with chronic use, causes a negative cognitive and affective state (emotions, mood, thoughts, etc.). These negative states motivate the patient to continue using the drug, as the individual remembers its reinforcing effect.
Psychological vicious circle. The use of a psychoactive substance also causes general psychological problems: a decrease in self-esteem, a deterioration in self-understanding, a distortion of identity, the emergence of insecurity, anger and self-pity, low tolerance for frustration, fear and fear, loss of meaning in life. These phenomena also lead to increased cravings for drug use.
Social vicious circle. Finally, the social sphere of addicts suffers. There is a violation of interpersonal relations, the skills necessary for resolving various difficulties and conflicts, as well as maintaining intimate relationships, are lost. Close people also suffer. There are problems with the law, at work, financial difficulties, a decrease in social status and, in the end, its loss.
Example. The therapist helped Karl identify the causative agents that caused him to drink alcohol. Karl was influenced by environmental factors, feeling tired and exhausted, and the quality of his marriage. All these factors to the greatest extent determined the development of his dependence. Karl felt the urge to drink when Maria - his wife - pressed on him, made some remark, demanded that he be responsible and spend more time with her and with the children. Karl felt panic attacks at the thought that he would not be able to drink alcohol. When Karl had problems, he turned to his mother for help, borrowed money from her, refusing to take responsibility. He wanted to continue his parasitic lifestyle, avoiding any changes.
Supportive factors
Among the main supporting factors, we note the following.
Physical addiction. Over time, the human body gets used to the drug and can no longer do without it. The absence of a narcotic substance causes sensations in the body, which grow from slight discomfort to severe pain, which prompts a person to use again.
Psychological addiction. Often, the drug becomes for an individual a specific strategy of behavior, with the help of which he cope with his problems in the family, at work, in social interactions, and other areas. This, in turn, develops a certain behavioral habit in the patient and, accordingly, behavioral dependence.
Social environment. Often, addicted people select a certain circle of friends, consisting of the same addicts, and are removed from other social interactions. To give up drugs also means to give up a social group.
Macro environment. The use of certain drugs can be supported by the macro environment and legislation. A prime example is television ads for alcohol and tobacco. In a number of countries, the use of heavier drugs is allowed.
Modulating factors
The main modulating factors for dependent patients can be noted. However, they will rather relate to the possibility of breakdown and relapse, in a patient who has refused to use, rather than in an actually dependent patient, since the state of the latter will be largely determined by supporting factors.
The physical condition of the patient. This factor should rather be considered within the framework of medical intervention, when the intake of the main drug is replaced by one or another medical means, after which the patient's craving for taking the drug subsides.
The patient's financial situation. Oddly enough, this factor can also affect drug intake. If the patient does not have enough money, and the drug is expensive, he will most likely refrain from taking it for some time. This can also include the availability of drugs.
The level of frustration. As noted above, for patients, taking a narcotic drug often acts as a way to solve one or another of their problems. Often, patients are able to abstain from using if everything else is in order, however, as soon as such a patient experiences stress, most likely he will turn to the drug again.
Social context. Many people are able to abstain from drug use where no one else is using it. However, as soon as, for example, an alcoholic gets into the company of drinking companions or just on a holiday where alcoholic beverages are used, he breaks down under the pressure of society. An individual can also be influenced by his relatives, who lend him money, solve problems for him, thereby, although not willingly, supporting his illness.
Addiction treatment
Addiction treatment is one of the most difficult areas of therapy, which requires a systematic approach to the disease. As a rule, it is necessary to combine a number of areas: pharmacological, psychotherapeutic, social, and behavioral. The effectiveness of addiction treatment is extremely low. The main approach that has proven itself in this vein is the 12 Steps program. Other programs are also used, for example, harm reduction, group reinforcement therapy, treatment by strengthening motivation, prevention of relapse, in some cases when addictions are accompanied by phobic symptoms, then hypnotherapy is most effective. Moreover, all these programs usually include elements of cognitive-behavioral therapy.
© You can find out more about the treatment of phobias and the psychological component of addiction on the website of the psychologist, hypnotherapist Gennady Ivanov.
Found a mistake in the text? Select it and press Ctrl + Enter.