- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Cardiac asthma
Brief description of the disease

Cardiac asthma is a complication of hypertension, atherosclerotic cardiosclerosis, heart attack, heart defects.
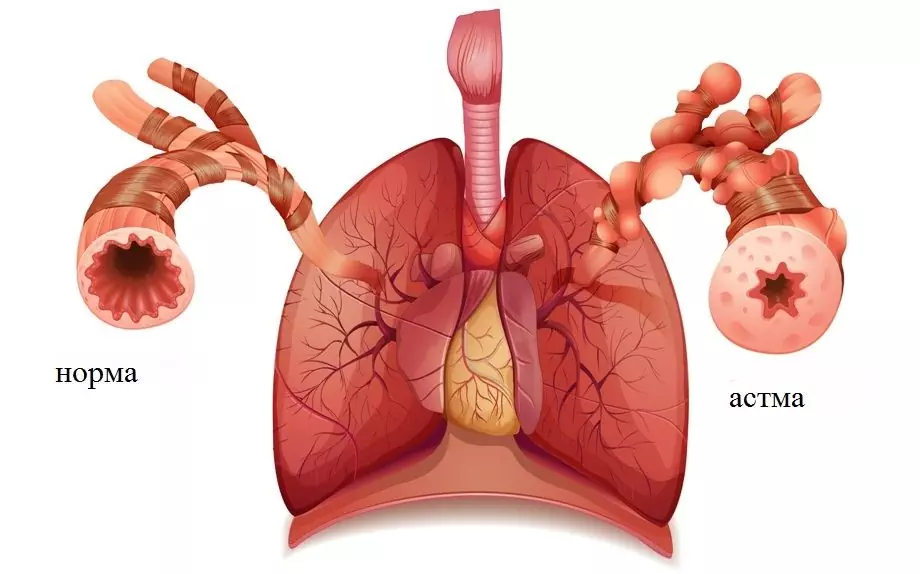
Cardiac asthma looks like an attack of shortness of breath and suffocation, provoked by stagnation of blood in the pulmonary vessels, the difficulties of its outflow into the left cardiac ventricle.
Reasons for the appearance
Cardiac asthma develops due to narrowing of the left atrioventricular orifice or left ventricular heart failure in myocarditis, acute infarction, extensive cardiosclerosis, aortic heart defects, mitral valve insufficiency, left ventricular aneurysm, paroxysmal large rises in pressure, accompanied by excessive left ventricular tension.
The cause of an attack in the daytime is usually emotional or physical stress, increased pressure, angina pectoris. In rare cases, asthma occurs after drinking or eating, but more often the attack develops at night, during sleep.
Symptoms of cardiac asthma
The main symptom of cardiac asthma is paroxysmal dyspnea, in which prolonged noisy inhalation prevails.
Symptoms of cardiac asthma occurring during the day: palpitations, chest tightness just before the attack.
If asthma develops at night, the patient wakes up from lack of air, shortness of breath, chest tightness, dry cough. Sweat appears on the face, the patient experiences anxiety and fear. During an attack, they usually breathe through the mouth, it is difficult to talk, there is a tangible need for oxygen.
Diagnosis of the disease
Diagnosis during an attack is made by assessing the symptoms of cardiac asthma. Differential diagnosis with bronchial asthma is of great importance (especially in the elderly).
Establishing the origin of asthma is very important because when providing emergency care for cardiac asthma, completely different medicines are used to relieve an attack that are not used in bronchial asthma.
The doctor must listen to the patient's heart. For this type of asthma, a gallop rhythm is characteristic, an accent is heard above the pulmonary trunk. The pulse may be weak, tachycardia may develop, exhalation is not difficult and distant wheezing is heard. Deviations can be seen on the ECG: coronary insufficiency, rhythm disturbance is noticeable.
With typical symptoms, it is not difficult to diagnose cardiac asthma, but if bronchospasm is present, the patient or his friends are questioned about the patient's predisposition to allergies, the presence of chronic bronchitis or other pulmonary diseases.
Treating cardiac asthma

Treatment begins with the provision of emergency care for cardiac asthma, which is primarily aimed at reducing the excitability of the respiratory center, the load on the small circle of blood flow. To do this, a 1% morphine solution (or a 2% pantopon solution) with a 1% atropine solution is injected subcutaneously. If tachycardia is expressed (more than 100 beats / minute), instead of atropine, pipolfen, suprastin or diphenhydramine is administered - 1 ml into the muscle. If the patient's pressure is low, morphine (pantopon) is replaced with a solution of promedol 2%, which is injected subcutaneously. Supplement it with caffeine, camphor. Morphine should not be administered if the respiratory rhythm is disturbed, intermittent breathing, in which the frequency decreases, and when the origin of the attack remains unclear (with bronchial asthma, morphine should not be administered).
Bloodletting is used as an emergency treatment for cardiac asthma: 200-300 ml of blood is released. Do not bleed under reduced pressure. In this case, as well as if the veins are poorly expressed, or it is necessary to repeat bloodletting, tourniquets are applied to the legs, squeezing the veins (not arteries - the pulse must be felt). The tourniquets are kept for no more than 30 minutes, they are removed gradually, loosening at intervals of several minutes. The imposition of tourniquets is excluded if the patient has edema of the extremities, hemorrhagic diathesis, thrombophlebitis, heart attack, angina pectoris.
Also, stopping the attack, with a pulse of at least 60 beats / minute (and if the patient did not take a drug containing digitalis), a solution of strophanthin 0.05% - 0.5 ml is administered. The drug is usually injected immediately after bloodletting (if it was carried out), into the same needle. Often, the drug is supplemented with euphyllin - a remedy effective for mixed asthma with symptoms of cardiac and bronchial origin, with mitral stenosis. It is impossible to inject aminophylline at low pressure.
Treatment of cardiac asthma continues with measures to reduce pulmonary congestion. To do this, 40 mg of lasix (furosemide) or 50 g of uregit (ethacrine acid) are injected intravenously. Sometimes in patients with hypertension, atherosclerotic cardiosclerosis, a good effect is observed after taking nitroglycerin.
All stages of the treatment of cardiac asthma are carried out against the background of constant oxygen therapy. When the respiratory center is inhibited, camphor, lobelin, and cordiamine are administered. The patient is given maximum rest during an attack. It cannot be transported; all the necessary procedures for the treatment of cardiac asthma are carried out on the spot. Hospitalization is necessary only if the attack cannot be stopped.
Prevention of the disease
To effectively prevent an attack, urgent and correct treatment of the underlying disease is necessary, which may include restriction of fluid, salt, taking diuretics, heart drugs.
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!