- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Bronchial asthma in children
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms of bronchial asthma in children
- Diagnostics
- Treatment of bronchial asthma in children
- Potential consequences and complications
- Forecast
- Prevention of bronchial asthma in children
Bronchial asthma in children is a chronic disease of the respiratory tract associated with hyperreactivity of the bronchi, that is, their increased sensitivity to irritants. The disease is widespread: according to statistics, approximately 7% of children suffer from it. The disease can manifest at any age and in children of any sex, but more often occurs in boys from 2 to 10 years old.

Bronchial asthma is a common chronic disease among children
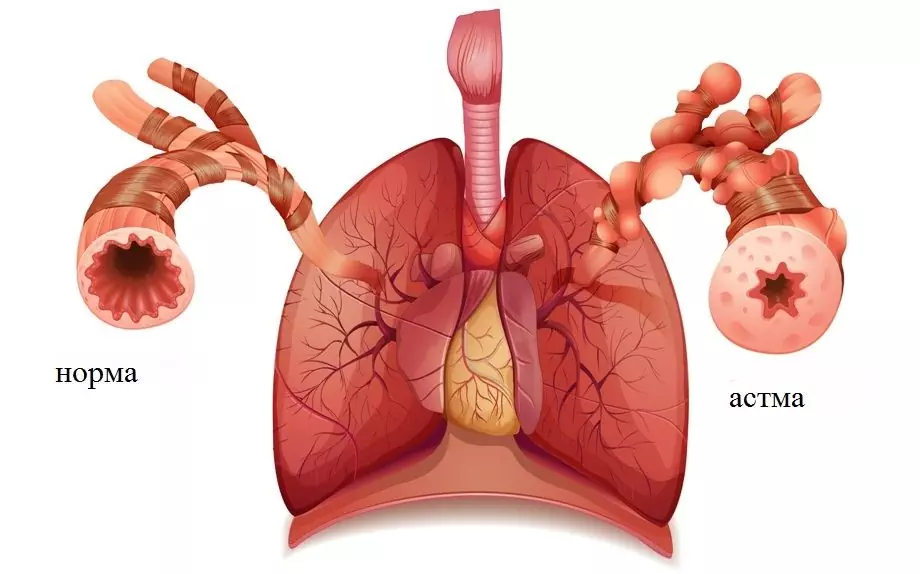
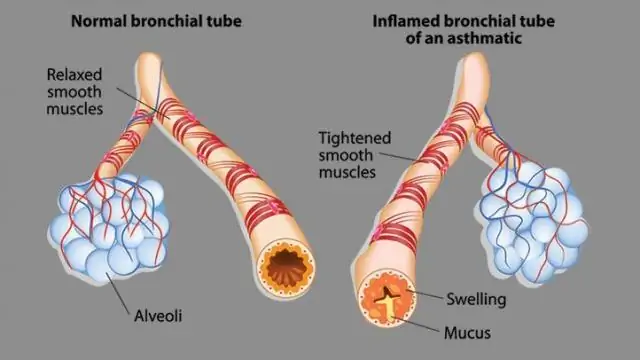
The main clinical sign of bronchial asthma in a child is recurrent attacks of shortness of breath or suffocation caused by widespread reversible bronchial obstruction associated with bronchospasm, mucus hypersecretion and mucosal edema.
In recent years, the incidence of bronchial asthma in children has been increasing everywhere, but especially in economically developed countries. Experts explain this by the fact that every year more and more artificial materials, household chemicals, industrial food products containing a large number of allergens are used. It should be borne in mind that the disease often remains undiagnosed, since it can be disguised as other pathologies of the respiratory system and, above all, as an exacerbation of chronic obstructive pulmonary disease (COPD).
Causes and risk factors
Risk factors for the development of bronchial asthma in children are:
- hereditary predisposition;
- constant contact with allergens (waste products of house dust mites, mold spores, pollen, proteins of dried urine and saliva, dandruff and pet hair, bird fluff, food allergens, cockroach allergens);
- secondhand smoke (inhalation of tobacco smoke).
Factors-provocateurs (triggers) that act on the inflamed bronchial mucosa and lead to the development of an attack of bronchial asthma in children are:
- acute respiratory viral infections;
- air pollutants such as sulfur or nitrogen oxide;
- β-blockers;
- non-steroidal anti-inflammatory drugs (Aspirin, Analgin, Paracetamol, Nurofen, etc.);
- pungent odors;
- significant physical activity;
- sinusitis;
- inhalation of cold air;
- gastroesophageal reflux.

Risk factors for the development of bronchial asthma in children
The formation of bronchial asthma in children begins with the development of a special form of chronic inflammation in the bronchi, which becomes the cause of their hyperreactivity, that is, increased sensitivity to the effects of nonspecific irritants. In the pathogenesis of this inflammation, the leading role belongs to lymphocytes, mast cells and eosinophils - cells of the immune system.
Hyperreactive inflamed bronchi respond to trigger factors by hypersecretion of mucus, spasm of bronchial smooth muscles, edema and mucosal infiltration. All this leads to the development of obstructive respiratory syndrome, which is clinically manifested by an attack of suffocation or shortness of breath.
Forms of the disease
According to the etiology, bronchial asthma in children can be:
- allergic;
- non-allergic;
- mixed;
- unspecified.
As a special form, doctors distinguish aspirin bronchial asthma. For her, the trigger factor is the child's intake of non-steroidal anti-inflammatory drugs. It is often complicated by the development of status asthmaticus.
Depending on the severity, there are several types of clinical course of bronchial asthma in children:
- Light episodic. The attacks occur less than once a week. In the interictal period, there are no signs of bronchial asthma in the child, and the lung function is not impaired.
- Light persistent. Attacks occur more often than once a week, but not daily. During an exacerbation, the child's sleep is disturbed, normal daily activity worsens. Spirometry indicators are normal.
- Moderately heavy. Choking attacks occur almost daily. As a result, the activity and sleep of children is significantly affected. To improve their condition, they need the daily use of inhaled β-antagonists. Spirometry indicators are reduced by 20-40% of the age norm.
- Heavy. Asthma attacks occur several times a day, often at night. Frequent exacerbations cause impaired psychomotor development of the child. Respiratory function indicators are reduced by more than 40% of the age norm.

The state of the respiratory tract in bronchial asthma
Symptoms of bronchial asthma in children
Choking or shortness of breath in children with bronchial asthma can occur at any time of the day, but most often they occur at night. The main symptoms of bronchial asthma in children:
- an attack of expiratory dyspnea (difficulty exhaling) or suffocation;
- unproductive cough with sticky, hard-to-separate sputum;
- cardiopalmus;
- wheezing dry (buzzing) wheezing, intensifying at the moment of inhalation; they are heard not only during auscultation, but also at a distance and therefore they are also called distant wheezing;
- boxed percussion sound, the appearance of which is explained by the hyper-airiness of the lung tissue.

Unproductive cough and shortness of breath - symptoms of bronchial asthma in a child
Symptoms of bronchial asthma in children at the time of a severe attack become different:
- the amount of breathing sounds decreases;
- cyanosis of the skin and mucous membranes appears and grows;
- paradoxical pulse (an increase in the number of pulse waves at the time of exhalation and a significant decrease, up to complete disappearance at the time of inhalation);
- participation in the act of breathing of the auxiliary muscles;
- taking a forced position (sitting, resting his hands on the bed, back of a chair or knees).
In children, the development of an attack of bronchial asthma is often preceded by a period of precursors (dry cough, nasal congestion, headache, anxiety, sleep disturbance). The attack lasts from several minutes to several days.
If an attack of bronchial asthma continues in a child for more than six hours in a row, this condition is regarded as status asthmaticus.
After the resolution of an attack of bronchial asthma in children, thick and viscous sputum leaves, which leads to easier breathing. Tachycardia is replaced by bradycardia. Blood pressure decreases. The child becomes inhibited, lethargic, indifferent to the environment, and often falls asleep soundly.
In the interictal periods, children suffering from bronchial asthma may feel quite well.
Diagnostics
For the correct diagnosis of bronchial asthma in children, it is necessary to take into account the data of an allergic history, laboratory, physical and instrumental studies.
Laboratory research methods for suspected bronchial asthma in children include:
- general blood test (eosinophilia is often detected);
- microscopy of sputum (Charcot-Leiden crystals, Kurshman's spirals, a significant amount of epithelium and eosinophils);
- study of the gas composition of arterial blood.
Diagnosis of bronchial asthma in children includes a number of special studies:
- lung function tests (spirometry);
- setting skin tests to identify causal allergens;
- detection of bronchial hyperactivity (provocative tests with a suspected allergen, physical activity, cold air, hypertonic sodium chloride solution, acetylcholine, histamine);
- chest x-ray;
- bronchoscopy (extremely rare).

Spirometry allows you to investigate lung function in suspected bronchial asthma in children
Differential diagnosis is required with the following conditions:
- foreign bodies of the bronchi;
- bronchogenic cysts;
- tracheo- and bronchomalacia;
- obstructive bronchitis;
- obliterating bronchiolitis;
- cystic fibrosis;
- laryngospasm;
- acute respiratory viral infection.
Treatment of bronchial asthma in children
The main areas of treatment for bronchial asthma in children are:
- identification of factors causing exacerbation of bronchial asthma, and elimination or limitation of contact with triggers;
- basic hypoallergenic diet;
- drug therapy;
- non-drug rehabilitation treatment.
Drug therapy of bronchial asthma in children is carried out using the following groups of drugs:
- bronchodilators (stimulants of adrenergic receptors, methylxanthines, anticholinergics);
- glucocorticoids;
- stabilizers of mast cell membranes;
- leukotriene inhibitors.

Symptomatic drugs can quickly stop bronchospasm
In order to prevent exacerbations of bronchial asthma, children are prescribed basic drug therapy. Its scheme is largely determined by the severity of the course of the disease:
- mild intermittent asthma - short-acting bronchodilators (β-adrenergic agonists) if necessary, but not more often than 3 times a week;
- mild persistent asthma - daily cromalin sodium or inhalation glucocorticoids plus long-acting bronchodilators, if necessary, short-acting bronchodilators, but not more often 3-4 times a day;
- moderate asthma - daily inhalation of glucocorticoids in a dose of up to 2,000 mcg, prolonged-acting bronchodilators; if necessary, short-acting bronchodilators can be used (no more than 3-4 times a day);
- severe asthma - daily inhalation of glucocorticoids (if necessary, they can be prescribed in a short course in the form of tablets or injections), long-acting bronchodilators; for relief of an attack - short-acting bronchodilators.
Therapy for an attack of bronchial asthma in children includes:
- oxygen therapy;
- β-adrenergic agonists (Salbutamol) by inhalation;
- epinephrine hydrochloride subcutaneously;
- Eufillin intravenously;
- glucocorticoids inside.
The indications for hospitalization are:
- the patient belongs to a high mortality group;
- ineffectiveness of the treatment;
- development of status asthmaticus;
- severe exacerbation (forced expiratory volume in 1 second is less than 60% of the age norm).
In the treatment of bronchial asthma in children, it is important to identify and eliminate the allergen, which is the trigger factor. For this, it is often necessary to change the child's diet and lifestyle (hypoallergenic diet, hypoallergenic life, change of residence, parting with a pet). In addition, long-term antihistamines may be prescribed for children.

For effective treatment of bronchial asthma in a child, it is important to identify the allergen and eliminate it
If the allergen is known, but it is impossible to get rid of contact with it due to one reason or another, then specific immunotherapy is prescribed. This method is based on the introduction to the patient (parenteral, oral or sublingual) of gradually increasing doses of the allergen, which reduces the body's sensitivity to it, that is, hyposensitization occurs.
During the period of remission, children with bronchial asthma are shown physiotherapy:
- speleotherapy;
- breathing exercises;
- acupressure;
- chest massage;
- hydrotherapy;
- ultraphonophoresis;
- electrophoresis;
- magnetotherapy;
- UHF therapy;
- inductothermy;
- aeroionotherapy.
Potential consequences and complications
The main complications of bronchial asthma are:
- asthmatic status;
- pneumothorax;
- pulmonary heart.
In children suffering from a severe form of the disease, glucocorticoid therapy can be accompanied by the development of a number of side effects:
- violation of water and electrolyte balance with the possible appearance of edema;
- increased blood pressure;
- increased excretion of calcium from the body, which is accompanied by increased fragility of bone tissue;
- an increase in blood glucose concentration, up to the formation of steroid diabetes mellitus;
- increased risk of occurrence and exacerbation of gastric ulcer and duodenal ulcer;
- decrease in the regenerative capacity of tissues;
- increased blood clotting, which increases the risk of thrombosis;
- decreased resistance to infections;
- obesity;
- moon face;
- neurological disorders.
Forecast
The prognosis for life in children with bronchial asthma is generally favorable. After puberty, attacks of bronchial asthma stop in 20-40% of children. The rest of the disease persists throughout their lives. The risk of death during a choking attack is increased in the following cases:
- a history of over three hospitalizations per year;
- a history of hospitalization in the intensive care unit;
- there have been cases of mechanical ventilation (artificial lung ventilation);
- an attack of bronchial asthma was at least once accompanied by loss of consciousness.
Prevention of bronchial asthma in children
The importance of preventing bronchial asthma in children cannot be overestimated. It includes:
- breastfeeding during the first year of life;
- gradual introduction of complementary foods in strict accordance with the age of the child;
- timely active treatment of respiratory diseases;
- keeping the home clean (wet cleaning, rejection of carpets and soft toys);
- refusal to keep pets (if any, careful observance of hygiene rules);
- preventing children from inhaling tobacco smoke (secondhand smoke);
- regular sports;
- annual vacation on the seaside or in the mountains.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!