- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Chronic colitis
The content of the article:
- Causes and risk factors
- Forms of chronic colitis
- Chronic colitis symptoms
- Diagnostics
- Chronic colitis treatment
- Possible complications and consequences
- Forecast
- Prevention
Chronic colitis is a set of long-term, undulating diseases of different parts of the colon, accompanied by morphologically confirmed inflammatory and dystrophic changes in its mucous membrane, impaired functioning of the organ.
It is generally accepted that the phenomena of chronic colitis are present to one degree or another in at least half of patients with gastrointestinal diseases. This pathology is common on all continents, it occurs equally often in both men and women. Male patients seek medical help for chronic colitis more often after the age of 40; in women, the disease is more common in the age group from 20 to 60 years.
The greatest prevalence of the disease is noted in Europe and North America, however, the collective term "chronic colitis" is not used in Western medicine.
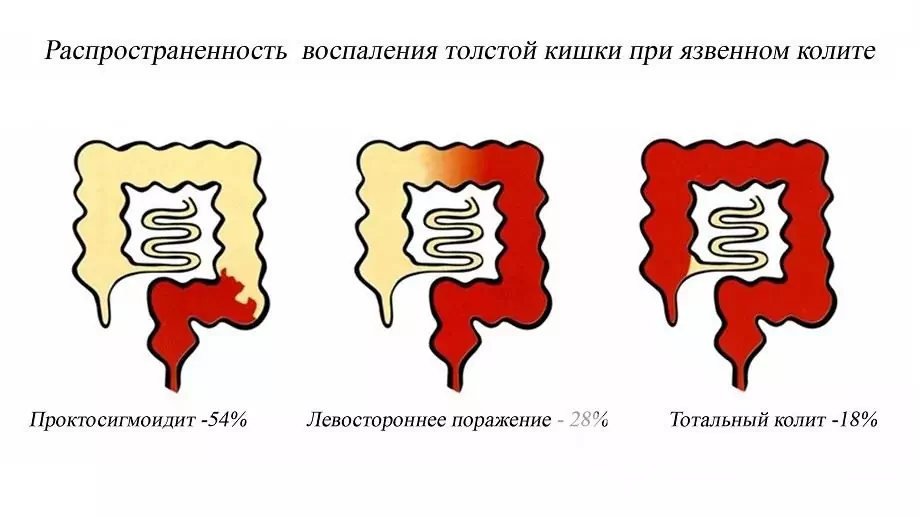
Localization options for the inflammatory process in chronic colitis
Causes and risk factors
The causes of chronic colitis are very diverse, the disease can be provoked by both pathogenic microorganisms and adverse effects of external physical factors, as well as internal causes.
Causal factors for the development of chronic colitis:
- infectious process (infection with bacterial agents (usually - Shigella, Salmonella, Yersinia, less often - Clostridia, Campylobacter), viruses (entero- and rotaviruses), protozoa (Giardia, amoeba, balantidia, etc.), pathogenic fungi, helminths);
- activation of its own opportunistic microflora;
- systematic gross violations of the diet;
- chronic diseases that contribute to the development of endogenous intoxication (chronic renal failure, liver failure, decompensated diabetes mellitus, thyrotoxicosis, etc.);
- chronic exogenous intoxication with heavy metal salts, pesticides, alkalis, alcohol and other aggressive substances;
- long-term food allergy;
- chronic coprostasis;
- exposure to ionizing radiation;
- congenital pathology of enzyme systems;
- long-term use of drugs that irritate the wall of the large intestine (salicylates and other non-steroidal anti-inflammatory drugs, laxatives, etc.).
Risk factors for chronic colitis:
- the presence of severe chronic diseases;
- industrial contact with toxic substances;
- immunodeficiency states;
- prolonged dysbiosis;
- autonomic dysfunction (violation of the innervation of the intestinal wall);
- antibacterial treatment;
- chronic alcoholic illness;
- postponed acute infectious and inflammatory diseases of the gastrointestinal tract;
- the presence of masses, adhesions and other mechanical factors that impede the passage of the contents of the large intestine;
- food stereotype with a small amount of fiber, liquid in the diet, the use of large quantities of processed meat, soft bread, seasonings, sauces, fatty, fried, spicy foods;
- atherosclerotic disease (ischemia of the mucous membrane of the large intestine);
- abuse of laxatives, enemas.

Antibiotic therapy, abuse of laxatives can lead to exacerbation of chronic colitis
A significant role in the development of chronic colitis is assigned to autoimmune aggression, when, against the background of active inflammation, the production of antibodies to the structural elements of the mucous membrane of the large intestine is activated, aggravating the pathological process.
In most cases, with chronic colitis in a patient, it is possible to establish a combination of several causal factors that mutually reinforce each other's action. Nevertheless, in some patients it is not possible to reliably establish the root cause of the disease, in this case they speak of cryptogenic colitis.
Forms of chronic colitis
Depending on the etiological factor, chronic colitis is subdivided as follows:
- infectious (viral, bacterial, mycotic);
- parasitic;
- alimentary (food-grade);
- intoxication (a consequence of exposure to both internal and external toxins);
- ischemic (impaired blood supply to the wall of the large intestine);
- radiation;
- medication;
- mechanical;
- allergic;
- mixed etiology;
- cryptogenic (with an unknown cause).
Depending on the localization of the inflammatory process:
- total, or pancolitis;
- segmental (with the localization of inflammation in a certain part of the large intestine: typhlitis (cecum and vermiform appendix), transversitis (transverse colon), sigmoiditis (sigmoid colon), proctitis (rectum).
In accordance with the morphological picture of mucosal lesions:
- catarrhal;
- erosive;
- ulcerative;
- atrophic;
- mixed.
Depending on the severity of the inflammatory process, chronic colitis can occur in mild, moderate and severe forms with a constant, recurrent or intermittent course of the disease.
By the presence of impaired motor function or manifestations of dyspepsia, 2 forms of chronic colitis are distinguished:
- with motor dysfunction (hyper- and hypokinetic forms);
- with dyspepsia (fermentative or putrid).
Chronic colitis symptoms
Local manifestations of the disease are the main ones in the clinical picture of chronic colitis:
- diarrhea (from 4-5 to 15 times a day with a severe form of the disease), in some cases it is possible to alternate diarrhea with constipation;
- the urge to defecate (possibly false) occurs against the background of a sharp change in body position (bending, jumping), after eating (the so-called snack symptom, more pronounced with transverse), under the influence of stress influences, in the early morning hours ("alarm chair" proctosigmoiditis);
- painful sensations, discomfort before or after the act of defecation;
- recurring dull, aching or sharp cramping pain in the abdomen (over the entire surface or in the lower part), aggravated by eating foods high in fiber, dairy products, fatty, fried foods, carbonated drinks, etc., decreasing or completely stopping after passing gas or defecation;
- decreased appetite;
- episodes of vomiting, single or repeated;
- weight loss;
- bloating, rumbling;
- feeling of incomplete emptying of the intestines after a bowel movement;
- belching with air, sometimes with the smell of rotten eggs;
- bitterness in the mouth;
- nausea;
- copious impurities of mucus in the feces;
- intestinal crises, characterized by a series of urgent urges to defecate with the release of normal feces at first, and then more liquid stool, often with an admixture of clear mucus, accompanied by cramping pains that stop after bowel movement.

Chronic colitis manifestations
In addition to local manifestations, there are general symptoms of chronic colitis:
- deterioration in general health;
- decreased performance;
- irritability, emotional instability;
- decreased tolerance to habitual physical activity;
- fast fatiguability;
- violation of sleep and wakefulness (sleepiness during the day, insomnia at night).
An exacerbation of chronic colitis is accompanied by an increase in symptoms, which during the period of remission may be practically absent or mild. Exacerbations are often provoked by errors in the diet, psychoemotional or physical overstrain, exacerbation of concomitant chronic pathology.
The characteristic of painful sensations depends on the localization of the inflammatory process: with typhlitis, pain is determined in the right iliac region, with sigmoiditis - in the left, with proctitis - in the projection of the rectum.
Diagnostics
The diagnosis of chronic colitis is based primarily on the characteristic clinical picture.
Physical examination data, laboratory and instrumental research methods, indicating the presence of chronic colitis:
- painfulness on palpation, a characteristic form of a spasmodic, inflamed intestine in the form of a dense cord, a drum sound during percussion over the lesion site are objectively determined;
- an increase in the number of leukocytes and an acceleration of ESR in a general blood test during an exacerbation of chronic colitis;
- during scatological examination, undigested fiber, starch grains, iodophilic microflora (during fermentation processes) or the remnants of undigested striated muscle fibers (during putrefactive processes), mucus are found in feces;
- endoscopic signs of inflammation, dystrophy and atrophy of the colon are detected (sigmoidoscopy, colonofibroscopy);
- when carrying out an X-ray study with a contrast agent, the smoothing of the structure of the mucous membrane, the disappearance of the haustra (symptom of a "water pipe") are noted.

Chronic colitis: results of irrigoscopy
Chronic colitis treatment
Drug therapy for chronic colitis:
- intestinal antiseptics;
- with indomitable diarrhea - enveloping, astringent preparations, sorbents;
- for constipation - laxatives (stimulating intestinal secretion, increasing the volume of feces, softening and lubricating agents), the drug of choice is lactulose;
- defoamers for flatulence;
- enzyme preparations;
- prokinetics if necessary;
- selective antispasmodics.
In addition to the drug effect, a significant role in treatment is played by adherence to a special diet for chronic colitis:
- limiting carbohydrates and dairy products;
- frequent, fractional meals;
- with persistent diarrhea - the exclusion of legumes, foods rich in fiber;
- with constipation - drinking a lot of water (at least 2 liters per day), foods high in fiber that stimulate peristalsis;
- refusal from fried, spicy, spicy, fatty foods.

With exacerbation of chronic colitis, diet 4a is indicated
During the period of exacerbation of chronic colitis, diet No. 4a is recommended (stale white bread, low-fat weak broths, steamed dishes of meat and fish, mashed porridge in water, soft-boiled eggs, steam omelets, jelly, decoctions and jelly from blueberries, bird cherry, pears, quince, rose hips, tea, coffee and cocoa on water).
Possible complications and consequences
Complications of chronic colitis can be:
- solarium (damage to the solar plexus);
- mesenteric adenitis (inflammation of the mesenteric lymph nodes);
- coprostasis (stagnation of feces);
- dysbiosis.
Forecast
With timely diagnosis, complex treatment and strict adherence to dietary recommendations, the prognosis is favorable.
Prevention
In order to prevent the development of chronic colitis, it is recommended:
- timely treatment of acute intestinal diseases;
- adherence to a rational diet;
- compliance with safety measures when working in hazardous production;
- avoiding alcohol abuse.
YouTube video related to the article:

Olesya Smolnyakova Therapy, clinical pharmacology and pharmacotherapy About the author
Education: higher, 2004 (GOU VPO "Kursk State Medical University"), specialty "General Medicine", qualification "Doctor". 2008-2012 - Postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty "Pharmacology, Clinical Pharmacology"). 2014-2015 - professional retraining, specialty "Management in education", FSBEI HPE "KSU".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!