- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Lumbar osteochondrosis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Lumbar osteochondrosis symptoms
- Diagnostics
- Treatment of lumbar osteochondrosis
- Therapeutic exercises for lumbar osteochondrosis
- Potential consequences and complications
- Forecast
- Prevention
Lumbar osteochondrosis is a chronic disease that develops as a result of a degenerative-dystrophic process in the intervertebral discs. The disease is widespread and affects most people between 25 and 40 years of age. According to statistics, back pain is experienced by every second adult at least once in their life, while in 95% of cases they are caused by osteochondrosis of the spine.
Lumbar osteochondrosis is a serious medical and social problem, since the disease mainly affects people of the most working age, and in addition, in the absence of treatment, it can cause the formation of a herniated disc.

Source: opesijas.ru
Causes and risk factors
Factors predisposing to the development of lumbar osteochondrosis are:
- anomalies in the structure of the spine;
- lumbarization - congenital pathology of the spine, characterized by the separation of the first vertebra from the sacrum and its transformation into the sixth (additional) lumbar;
- sacralization is a congenital pathology in which the fifth lumbar vertebra is fused with the sacrum;
- asymmetric arrangement of the joint spaces of the intervertebral joints;
- pathological narrowing of the spinal canal;
- reflected spondiogenic pain (somatic and muscle);
- obesity;
- sedentary lifestyle;
- prolonged exposure to vibration;
- systematic physical stress;
- smoking.
Unfavorable static-dynamic loads in combination with one or several risk factors lead to a change in the physiological properties of the nucleus pulposus of the fibrous disc, which plays a cushioning role and ensures the mobility of the spinal column. This process is based on the depolymerization of polysaccharides, which leads to the loss of moisture in the tissue of the gelatinous core. As a result, the nucleus pulposus, and with it the fibrous disc, lose their elastic properties. Further mechanical stress provokes protrusion of the annulus fibrosus that has lost its elasticity. This phenomenon is called protrusion. Cracks appear in the fibrous nucleus, through which fragments of the nucleus pulposus fall out (prolapse, herniated disc).
Instability of the spinal segment is accompanied by reactive changes in the bodies of adjacent vertebrae, intervertebral joints, and concomitant spondyloarthrosis develops. Significant muscle contraction, for example, against the background of physical activity, leads to a displacement of the vertebral bodies and entrapment of the nerve roots with the development of radicular syndrome.
Another cause of pain and neurological symptoms in lumbar osteochondrosis can be osteophytes - bone outgrowths on the processes and vertebral bodies that cause radicular syndrome or compression myelopathy (spinal cord compression).
Forms of the disease
Depending on which structures are involved in the pathological process, lumbar osteochondrosis is clinically manifested by the following syndromes:
- reflex - lumbodynia, lumboishalgia, lumbago; develop against the background of reflex overstrain of the back muscles;
- compression (spinal, vascular, radicular) - compression (compression) of the spinal cord, blood vessels or nerve roots leads to their development. Examples are lumbosacral radiculitis, radiculoischemia.
Lumbar osteochondrosis symptoms
With lumbar osteochondrosis, the symptoms are determined by which structures are involved in the pathological process.
Lumbago occurs under the influence of hypothermia or physical overstrain, and sometimes for no apparent reason. The pain appears suddenly and is of a shooting character. It intensifies when sneezing, coughing, turning the body, exercising, sitting, standing, walking. In the supine position, the pain sensations are significantly weakened. Sensitivity and reflexes are preserved, the range of motion in the lumbar spine is reduced. On palpation observe:
- soreness in the lumbar region;
- spasm of the paravertebral muscles;
- flattening of the lumbar lordosis, which in many cases is combined with scoliosis.
Nerve root tension syndrome with lumbago is negative. When raising a straight leg, patients note an increase in pain in the lumbar region, and not their appearance in an extended lower limb.
With lumbodynia, the clinical picture resembles lumbago, however, an increase in the intensity of pain occurs over several days.
With lumboishalgia, patients complain of pain in the lumbar region, which radiates to one or both lower extremities. The pain spreads to the buttocks and back of the thigh and never reaches the feet. For lumboishalgia, vasomotor disorders are characteristic:
- changes in temperature and color of the skin of the lower extremities;
- feeling hot or chilly;
- violation of blood circulation.
The development of lumbar compression syndromes is clinically manifested by the following symptoms:
- dermatomal hypalgesia;
- shooting pains;
- weakening or complete loss of deep reflexes;
- peripheral paresis.
With compression syndromes, pain increases with bending of the trunk, sneezing and coughing.
Diagnostics
Diagnosis of lumbar osteochondrosis is carried out on the basis of data on the clinical picture of the disease, laboratory and instrumental research methods.
In blood tests against the background of lumbar osteochondrosis, the following may be noted:
- decrease in calcium concentration;
- increased ESR;
- increased levels of alkaline phosphatase.
In the diagnosis of lumbar osteochondrosis, X-ray examination of the spine is of great importance.
X-ray signs that confirm the diagnosis are:
- change in the configuration of the affected segment;
- pseudospondylolisthesis (displacement of adjacent vertebral bodies);
- deformation of the closing plates;
- flattening of the intervertebral disc;
- unequal height of the intervertebral disc (a symptom of a spacer), which is associated with asymmetric muscle tone.

Source: sustavrip.ru
Also, in the diagnosis of lumbar osteochondrosis, if indicated, are used:
- myelography, computed or magnetic resonance imaging - are necessary for persistent symptoms, the development of neurological deficits;
- scintigraphy (study of the accumulation of phosphorus by the bone system, labeled with tech-99) - is performed if a tumor or infectious process is suspected, or spinal injury.
Differential diagnosis of lumbar osteochondrosis is carried out with the following diseases:
- spondylolisthesis;
- dyshormonal spondylopathy;
- ankylosing spondylitis (ankylosing spondylitis);
- infectious processes (disc inflammation, spinal osteomyelitis);
- neoplastic processes (primary tumor of the spine or its metastatic lesions);
- rheumatoid arthritis;
- deforming osteoarthritis of the hip joint;
- reflected pain (diseases of internal organs and large blood vessels).
Treatment of lumbar osteochondrosis
With lumbar osteochondrosis, the following treatment tactics are usually followed:
- bed rest for 2-3 days;
- traction of the affected segment of the spine;
- strengthening the back and abdominal muscles (creating the so-called muscle corset);
- impact on pathological myofascial and myotonic processes.
In most cases, conservative treatment of lumbar osteochondrosis is carried out, including the following measures:
- infiltration anesthesia of muscles with a solution of local anesthetics, for example, 2% novocaine solution;
- taking non-steroidal anti-inflammatory drugs;
- taking desensitizing agents;
- vitamin therapy;
- taking tranquilizers and antidepressants;
- manual therapy, massage;
- physiotherapy;
- acupuncture;
- post-isometric relaxation.
The absolute indications for surgical treatment of lumbar osteochondrosis are:
- acute or subacute spinal cord compression;
- development of cauda equina syndrome, characterized by dysfunction of the pelvic organs, sensory and motor disorders.
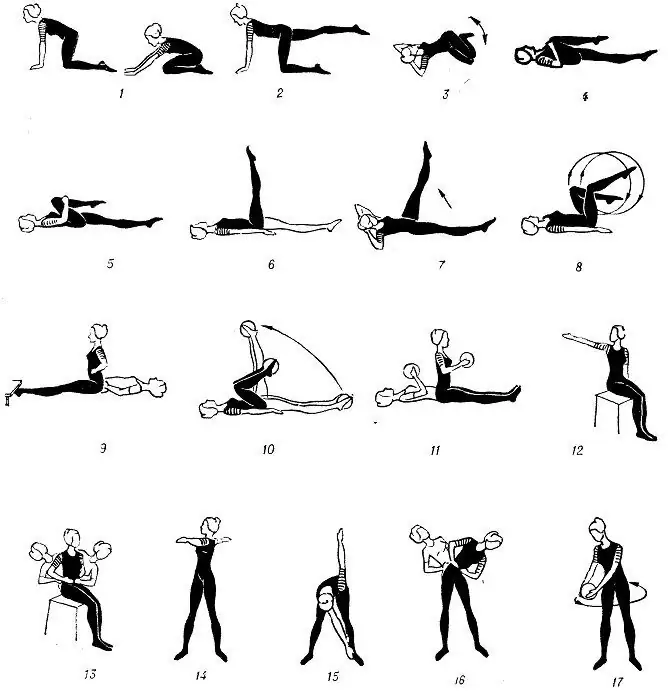
Therapeutic exercises for lumbar osteochondrosis
In the complex treatment of lumbar osteochondrosis, physical therapy plays a significant role. Regular exercises allow you to normalize the muscle tone of the paravertebral muscles, improve metabolic processes in the tissues affected by the pathological process, and in addition form a well-developed muscular corset that can support the spine in the correct position, remove unnecessary static loads from it.

Source: sustavzdorov.ru
In order for gymnastics with lumbar osteochondrosis to bring the greatest effect, the following principles should be adhered to:
- regularity of classes;
- a gradual increase in the intensity of physical activity;
- avoiding overwork during class.
Physiotherapy should be done under the guidance of an experienced instructor, who will select the exercises that are most effective for a particular patient and control the correctness of their implementation.
In addition to classes with an instructor, a complex of morning exercises should be performed daily, which includes special exercises for lumbar osteochondrosis.
- Relaxation and contraction of the abdominal muscles. The starting position is standing, feet shoulder-width apart, arms lowered to the body. Take a smooth breath, relaxing the muscles of the anterior abdominal wall. During exhalation, pull the stomach in as much as possible, straining the abdominal muscles. The exercise should be repeated until mild fatigue appears.
- Head movements with spinal flexion. The starting position is kneeling, resting on the floor with outstretched arms, the back is straight. Slowly raise your head and bend in your back. Hold in this position for a few seconds, and then smoothly return to the starting position. Repeat at least 10-12 times.
- "Pendulum". The starting position is lying on your back, arms along the body, legs bent at right angles at the knee and hip joints. Turn your legs to the right and left in swinging pendulum-like movements, trying to reach the floor. In this case, the shoulder blades cannot be torn off the floor.
- "Boat". The starting position is lying on your stomach, arms extended forward. Tear off the upper body and legs from the floor, bending in the back. Hold this position for 5-6 seconds and slowly return to the starting position. Run 10 times.
Potential consequences and complications
The main complications of lumbar osteochondrosis are:
- the formation of an intervertebral hernia;
- vegetative vascular dystonia;
- spondylolysis, spondylolisthesis;
- osteophytosis;
- spondyloarthrosis;
- stenosis of the spinal canal, which leads to compression of the spinal cord and can cause permanent disability and a decrease in the quality of life.
Prolonged compression of the nerve roots that innervate certain organs of the abdominal cavity over time leads to a deterioration in their functioning. As a result, patients have intestinal dysfunctions (constipation, diarrhea, flatulence) and pelvic organs (urinary disorders, erectile dysfunction, frigidity, infertility).
Forecast
Pain syndrome in lumbar osteochondrosis occurs in the form of remissions and exacerbations. Lumbago lasts 10-15 days, after which the patient's condition improves, the pain subsides. A favorable outcome can be prevented by the associated secondary diseases. Often, with lumbar osteochondrosis, there is a recurrence of pain attacks, which each time become more intense and prolonged.
Patients with severe lumbar osteochondrosis, with persistent pain and other manifestations are recognized as temporarily disabled. If their condition does not improve within four months, the issue of establishing a disability group is decided.
Prevention
Prevention of the development of osteochondrosis of the spine consists in the following measures:
- to give up smoking;
- normalization of body weight;
- improvement of the general physical condition, an active lifestyle;
- avoidance of provoking conditions (lifting weights, sudden movements, turns, tilts).
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!