- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Acute heart failure
The content of the article:
- Causes of Acute Heart Failure and Risk Factors
- Forms of the disease
- Stages
-
Symptoms of acute heart failure
- Acute left ventricular failure
- Acute right ventricular failure
- Diagnostics
- Treatment of acute heart failure
- Possible complications and consequences
- Forecast
- Prevention
Acute heart failure (AHF) is a condition that occurs as a result of a sharp weakening of the contractile function of the heart muscle, accompanied by stagnant processes in the pulmonary and systemic circulation, as well as a violation of intracardiac dynamics. Acute heart failure leads to extremely serious complications due to dysfunctions of internal organs due to the inability of the myocardium to provide the necessary blood supply.

Acute heart failure is the leading cause of hospitalization and mortality
The condition can occur as an exacerbation of chronic heart failure, or it can make its debut spontaneously in individuals without a history of cardiac dysfunction. Acute heart failure ranks first among the causes of hospitalization and in terms of mortality in many countries of the world.
Causes of Acute Heart Failure and Risk Factors
The reasons contributing to the onset of acute heart failure are conditionally divided into three groups:
- those that lead to an increase in cardiac output;
- those that lead to a sharp and significant increase in preload;
- those that lead to a sharp and significant increase in afterload.
Among them, the most common causes of acute heart failure are:
- aortic dissection;
- pulmonary embolism;
- heart defects (congenital and acquired);
- exacerbation of chronic heart failure;
- unstable angina;
- anemia;
- arrhythmias;
- hypertensive crisis;
- cardiac tamponade;
- complications of ischemic heart disease (heart attack, acute coronary syndrome);
- tense pneumothorax;
- overhydration;
- exacerbation of chronic obstructive pulmonary disease;
- cardiomyopathy in women during pregnancy;
- severe infectious diseases; and etc.
AHF can develop against the background of sepsis, thyrotoxicosis and other severe pathological conditions.
Acute heart failure of the left type (left ventricular) is formed in such pathologies when the load falls predominantly on the left ventricle: myocardial infarction, hypertension, aortic heart disease.
Acute heart failure of the right type (right ventricular) can be caused by exudative pericarditis, stenosis of the mouth of the pulmonary artery, adhesive pericarditis.
Forms of the disease
Due to the variety of reasons contributing to the onset of acute heart failure, it is classified depending on the prevailing lesions of certain parts of the heart and the mechanisms of compensation / decompensation.
By the type of hemodynamics:
- Acute heart failure with congestive hemodynamics.
- Acute heart failure with hypokinetic type of hemodynamics (cardiogenic shock, low ejection syndrome).
Stagnant, in turn, is divided into:
- acute heart failure of the left type (left ventricular, or left atrial);
- acute heart failure of the right type (right ventricular, or right atrial);
- total (mixed) acute heart failure.

The incidence of different types of acute heart failure
Hypokinetic (cardiogenic shock) is of the following types:
- true shock;
- reflex;
- arrhythmic.
According to the standards of the European Society of Cardiology (adopted in 2008), acute heart failure is divided into the following forms:
- exacerbation of chronic heart failure;
- pulmonary edema;
- cardiogenic shock;
- isolated right ventricular acute heart failure;
- acute heart failure in acute coronary syndrome;
- chronic heart failure with hypertension.
Stages
The severity classification is based on the assessment of peripheral circulation:
- class I (group A, "warm and dry");
- class II (group B, "warm and humid");
- class III (group L, "cold and dry");
- class IV (group C, "cold and wet").
Depending on the radiological signs and manifestations of acute heart failure (classification according to Killip), there are:
- class I - no signs of heart failure;
- class II - moist rales in the lower parts of the lungs, symptoms of impaired pulmonary circulation;
- class III - moist wheezing in the lungs, pronounced signs of pulmonary edema;
- class IV - cardiogenic shock, peripheral vasoconstriction, impaired renal excretory function, hypotension.
The Kilippe classification was developed to assess the condition of patients with acute heart failure, which developed against the background of myocardial infarction, but can also be used for other types of pathology.
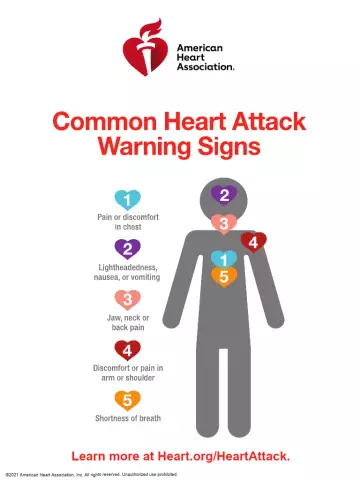
Symptoms of acute heart failure
In acute heart failure, patients complain of weakness, confusion. There is a pallor of the skin, the skin is moist, cold to the touch, there is a decrease in blood pressure, a decrease in the amount of urine excreted (oliguria), a threadlike pulse. Symptoms of the underlying disease may appear, against the background of which AHF has developed.
In addition, acute heart failure is characterized by:
- peripheral edema;
- soreness in the epigastric region on palpation;
- dyspnea;
- wet wheezing.
Acute left ventricular failure
Left-sided AHF manifestations are alveolar and interstitial pulmonary edema (cardiac asthma). Interstitial pulmonary edema develops more often against the background of physical and / or nervous tension, but it can also manifest itself during sleep in the form of sudden suffocation, provoking sudden awakening. During an attack, there is a lack of air, a hacking cough with characteristic shortness of breath, general weakness, pallor of the skin. Due to a sharp increase in shortness of breath, the patient takes a forced position, sitting with his legs down. Breathing hard, irregular pulse (gallop rhythm), weak filling.

Acute left ventricular failure presents with interstitial pulmonary edema (cardiac asthma)
With the progression of congestion in the pulmonary circulation, pulmonary edema develops - acute pulmonary insufficiency, which is caused by significant sweating of the transudate into the lung tissue. Clinically, this is expressed by suffocation, cough with the release of copious amounts of frothy sputum mixed with blood, wet wheezing, cyanosis of the face, nausea, and vomiting. The pulse is threadlike and the blood pressure drops. Pulmonary edema is a medical emergency that requires immediate intensive care due to the high probability of death.
Acute left ventricular failure may present with syncope due to cerebral hypoxia due to asystole or decreased cardiac output.
Acute right ventricular failure
Acute heart failure of the right type develops against the background of pulmonary embolism. Congestion in the systemic circulation is manifested by shortness of breath, cyanosis of the skin, edema of the lower extremities, intense pain in the heart and right hypochondrium. Blood pressure decreases, pulse is frequent, weak filling. There is an increase in the liver, as well as (less often) the spleen.

In acute right ventricular failure, patients complain of severe pain in the region of the heart and edema of the lower extremities
Signs of acute heart failure due to myocardial infarction range from mild pulmonary congestion to a sharp decrease in cardiac output and manifestations of cardiogenic shock.
Diagnostics
For the diagnosis of AHF, complaints and anamnesis are collected, during which the presence of diseases, against the background of which the pathology has developed, is clarified, with special attention to the drugs taken. Then they carry out:
- objective examination;
- auscultation of the heart and lungs;
- electrocardiography;
- echocardiography;
- stress tests based on electrocardiography (treadmill test, bicycle ergometry);
- X-ray examination of the chest organs;
- magnetic resonance imaging of the heart;
- general blood analysis;
- biochemical blood test (levels of glucose, electrolytes, creatinine, urea, hepatic transaminases, etc.);
- determination of blood gas composition.
If necessary, coronary angiography is performed, in some cases, an endomyocardial biopsy may be required.
To determine the lesion of internal organs, an ultrasound of the abdominal cavity is performed.
For the purpose of differential diagnosis of dyspnea in acute heart failure and dyspnea due to non-cardiac causes, natriuretic peptides are determined.
Treatment of acute heart failure
Patients with AHF should be admitted to a cardiac intensive care unit or an intensive care unit and intensive care unit.
The ambulance scheme at the prehospital stage for patients with acute heart failure of the left type includes:
- relief of attacks of the so-called respiratory panic (if necessary with the help of narcotic analgesics);
- inotropic stimulation of the heart;
- oxygen therapy;
- artificial ventilation of the lungs;
- reduction of pre- and afterload on the heart;
- decrease in pressure in the pulmonary artery system.

Treatment of acute heart failure is carried out in the cardiac intensive care unit
Urgent measures for stopping an attack of acute right ventricular failure include:
- elimination of the main reason, against the background of which a pathological condition arose;
- normalization of blood supply to the pulmonary vascular bed;
- elimination or reduction of the severity of hypoxia.
Treatment of acute heart failure in the cardiac intensive care unit is carried out under invasive or non-invasive continuous monitoring:
- invasive - catheterization of the peripheral artery or central vein (according to indications) is performed, with the help of the catheter, blood pressure, venous blood oxygen saturation is monitored, and medications are administered;
- non-invasive - blood pressure, body temperature, the number of respiratory movements and heartbeats, urine volume are monitored, an ECG is performed.
Therapy of acute heart failure in the cardiac intensive care unit is aimed at minimizing cardiac dysfunctions, improving blood parameters, optimizing blood supply to tissues and organs, as well as saturating the body with oxygen.
For the relief of vascular insufficiency, the introduction of fluid under the control of diuresis is used. With the development of cardiogenic shock, vasopressor agents are used. With pulmonary edema, diuretic drugs, oxygen inhalation, cardiotonic drugs are indicated.
Parenteral nutrition is indicated for the patient until the critical condition is overcome.
When transferring from the intensive care unit, the patient is rehabilitated. At this stage of treatment, the need for surgical interventions is determined.
The treatment regimen for acute heart failure is selected depending on the etiological factors, the form of the disease and the patient's condition and is carried out through oxygen therapy, as well as taking medications of the following main groups:
- loop diuretics;
- vasodilators;
- inotropic drugs; and etc.
Drug therapy is supplemented by the appointment of vitamin complexes, and a diet is shown to patients.
If acute heart failure has developed against the background of heart defects, heart aneurysms and some other diseases, the issue of surgical treatment is considered.
After discharge from the hospital, the patient's physical rehabilitation continues, and further monitoring of his health is carried out.
Possible complications and consequences
Acute heart failure is dangerous precisely because of the high risk of developing life-threatening conditions:
- cardiogenic shock;
- pulmonary edema;
- atrial fibrillation;
- atrioventricular block;
- thromboembolism.
Forecast
With cardiogenic shock, the mortality rate reaches 80%.
The five-year survival rate for patients with acute heart failure is 50%.
Long-term prognosis depends on the presence of concomitant diseases, the severity of the course of heart failure, the effectiveness of the treatment used, the general condition of the patient, his lifestyle, etc.
Timely adequate treatment of pathology in the early stages gives positive results and provides a favorable prognosis.
Prevention
In order to prevent the development, as well as to prevent the progression of already existing acute heart failure, it is recommended to adhere to a number of measures:
- timely consultations with a cardiologist in case of suspected cardiac pathology;
- sufficient physical activity (regular, but not exhausting);
- balanced diet;
- control of body weight;
- timely treatment and prevention of diseases that can lead to the onset of acute heart failure;
- rejection of bad habits.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!