- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Coxsackie virus
The content of the article:
- Causes and risk factors
- Forms of the disease
- Coxsackie virus symptoms
- Features of the course of the disease in children
- Diagnostics
- Treatment of Coxsackie virus infection
- Possible complications and consequences
- Forecast
- Prevention of the Coxsackie virus
Coxsackie virus (Coxsackievirus) is one of the representatives of enteroviruses that lives and multiplies in the digestive tract, but can infect other tissues and organs. The virus is resistant to freezing and the action of a number of disinfectants (ether, lysol, 70% ethyl alcohol). It remains viable in feces for more than six months. The Coxsackie virus in adults is diagnosed much less often than in children; children under 5 years of age are most susceptible to it. The infection can be transmitted from person to person; after the transferred disease, the patient has a tense type-specific immunity.

Coxsackie virus is an enterovirus that multiplies in the digestive tract
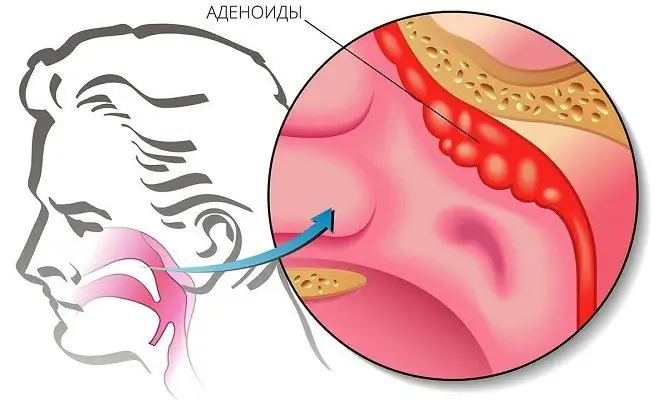
The virus is an intracellular parasite. The entrance gates of the infection are the mucous membranes of the pharynx and gastrointestinal tract. After entering the body, the primary replication of viral particles and their accumulation in the cells of the mucous membranes of the nasal cavity, pharynx, and small intestine occurs. Then the infectious agent enters the bloodstream and circulates for some time in the general bloodstream, as a result of which it can migrate to various organs and tissues, leading to the development of an inflammatory process in them. Different serotypes of the Coxsackie virus have different affinity for the tissues of the human body. The largest amount of the virus, as a rule, is localized in nerve cells, internal organs, striated muscles, skin. Depending on the serological type of the virus,as well as from the individual characteristics of the organism, the outcome of the disease can be a complete cure, the transition of the disease to a chronic form (with prolonged preservation of the infectious agent in the affected tissues and organs) or the carrier of viruses.
Inactivation of the Coxsackie virus occurs upon drying, exposure to ultraviolet radiation, heating to 50 ˚С, disinfection with a 0.3% formaldehyde solution or chlorine-containing preparations.
Causes and risk factors
The source of infection is a sick person or a virus carrier. Most often, infection with the Coxsackie virus occurs through contaminated food, water, and household items. The faecal-oral route of transmission is most common in young children. In addition, the Coxsackie virus can be transmitted by airborne droplets from a sick person to a healthy one. Transplacental transmission of the virus is also possible (i.e., from an infected mother to a fetus). In addition, cockroaches and flies can carry the virus.
Risk factors include childhood, old and old age, as well as immunodeficiency states.

Coxsackie virus is transmitted by airborne droplets and fecal-oral routes
In regions with a temperate climate, the peak incidence of infection caused by the Coxsackie virus occurs in the summer-autumn period.
Forms of the disease
Coxsackie viruses are divided into two groups:
- Group A - 24 serological types. Viruses of this group are localized in the skin, mucous membranes, and can cause acute hemorrhagic conjunctivitis, upper respiratory tract diseases, aseptic meningitis, enteroviral vesicular stomatitis, etc.
- Group B - 6 serotypes. These viruses infect the heart, pleura, liver, pancreas, can cause hepatitis, inflammation of the heart muscle (myocarditis), inflammation of the visceral and parietal layers of the pericardium (pericarditis), pericardial effusion, etc.
Some of the serotypes of group A, as well as all types of group B, are capable of multiplying in embryonic cell culture. Viruses of both groups have a common complement-binding antigen, some strains have hemagglutinating properties in relation to group O erythrocytes.
The infectious process caused by the Coxsackie virus can take the following forms:
- catarrhal;
- spinal (poliomyelitis-like);
- encephalic.
Coxsackie virus symptoms
The pathological processes that occur during infection with the Coxsackie virus are characterized by wide clinical polymorphism, however, in most cases, the disease is asymptomatic and sometimes completely asymptomatic.
The incubation period lasts several days. The first sign of the Coxsackie virus is an increase in body temperature to 39-40 ° C, while fever can persist for several days and / or proceed in waves. Patients have hyperemia of the skin of the face, injections of the sclera, moderate hyperemia of the mucous membrane of the oropharynx. If the upper respiratory tract is affected, a sore throat, nasal discharge, and coughing appear. Patients complain of weakness, fatigue, headache. Due to damage to the mucous membrane of the pharynx, eating can be difficult. In some cases, there is pain in the abdomen (mainly in the right iliac region), swelling, repeated vomiting, diarrhea, rashes on the upper and lower extremities, as well as on the face and chest. In the standard, uncomplicated course of the disease, symptoms are usuallydisappear within 1-2 weeks.

The first symptom of the Coxsackie virus is an increase in body temperature to 39-40 ˚С
The Coxsackie virus can cause sore throat. In this case, there is a reddening of the palatine arches and tonsils against the background of pronounced signs of intoxication of the body. Later, rashes appear on the affected areas of the mucous membrane. Elements of the rash burst, forming areas of erosion with a hyperemic rim, covered with a grayish coating. Rashes and erosion are prone to merging with each other.
With the development of epidemic myalgia, patients experience bouts of muscle pain. Painful sensations arise in the muscles of the chest, abdomen, upper and lower extremities. Myalgia of the chest muscles causes difficulty breathing. Pain in the muscles of the anterior abdominal wall can mimic the clinical picture of an acute abdomen. Muscle pains bother the patient for several days, and then subside, however, recurrence of myalgia also occurs.
The development of viral meningitis is manifested by positive meningeal symptoms (stiff neck muscles, photophobia, positive Kernig and Brudzinsky symptoms, intense headache), lethargy, apathy, in some cases - increased sensitivity to sounds, convulsions, psycho-emotional excitement. Consciousness in patients is usually preserved.
With viral conjunctivitis (it can be catarrhal or hemorrhagic), there is a sharp pain in the eyes, watery eyes, a feeling of a foreign body in the eyes. The conjunctiva is hyperemic, the eyelids are edematous, hemorrhages in the sclera may be noted. Usually one eye is affected first, then the second is involved in the pathological process.
Patients who have suffered an acute illness caused by the Coxsackie virus can remain infectious for another two months after the symptoms of the disease have completely disappeared, and in the case of a chronic form of infection - a year or more.
Features of the course of the disease in children
Coxsackie virus does not occur in children under three months of age, with the exception of newborns who become infected intrauterinely or during childbirth.
The disease in childhood is usually more severe than when infected with the Coxsackie virus in adults.
The incubation period is 2 to 10 days. The clinical picture depends on the location of the infectious agent.
In children 3-10 years old, the disease usually proceeds in the form of tonsillitis. The prodromal period (from 3 to 6 days) is characterized by decreased appetite, moodiness, lethargy. Then a sore throat occurs, the body temperature rises, small vesicular rashes form on the mucous membrane of the oropharynx, the cervical lymph nodes increase in size and become painful on palpation.

In children 3-10 years old, the Coxsackie virus often occurs in the form of a sore throat
In children under two years of age, when infected with the Coxsackie virus, an intolerance to dairy products (diarrhea, nausea and vomiting when consumed) may appear.
The most severe is encephalomyocarditis of newborns caused by the virus. Children have severe weakness, drowsiness, anorexia, vomiting and shortness of breath may occur. The skin becomes cyanotic, the liver increases in size, and tachycardia occurs. The disease can occur with or without an increase in body temperature. With encephalomyocarditis of newborns, the risk of developing convulsive syndrome and coma is high.
Diagnostics
Diagnosis is based on the presence of typical clinical manifestations (tonsillitis, encephalomyocarditis of newborns, epidemic myalgia, etc.). In this case, the seasonality (summer-autumn period) and the epidemic situation in the region are important. During the collection of complaints and anamnesis, attention is paid to possible contacts of the patient with carriers of the infection. Additional studies are prescribed depending on the damage by the virus to certain organs and tissues.

The easiest way to diagnose the Coxsackie virus is to detect antibodies to it
Direct isolation of an infectious agent from biological fluids (blood, feces, cerebrospinal fluid, discharge from the nasopharynx, lacrimal fluid) of a sick person is possible, but rarely performed in clinical practice. More often they use another method - the detection of antibodies to the virus, for which they use the complement binding reaction and the hemagglutination inhibition reaction. The diagnostic criterion is an increase in antibody titer by four or more times. In addition, the infectious agent can be detected in the patient's feces and nasopharyngeal washes using the polymerase chain reaction, which also makes it possible to determine the genotype of the virus.
Treatment of Coxsackie virus infection
Often, the patient self-heals within a week from the moment the first symptoms of the disease caused by the Coxsackie virus appear.
Etiotropic treatment of the Coxsackie virus has not been developed. Therapy consists in carrying out detoxification measures, as well as eliminating the symptoms of the disease.
Analgesic, anti-inflammatory and sedative drugs, as well as enterosorbents are prescribed. When rashes and ulcerations appear on the skin and mucous membranes, local antiseptic preparations are used. With severe itching in the affected areas, antihistamines are indicated.

Coxsackie virus treatment is mostly symptomatic
In a severe course of the disease with involvement of the nervous system in the pathological process, corticosteroids are indicated, in some cases - diuretic drugs. In the event of the development of life-threatening conditions, a complex of resuscitation measures and intensive therapy may be required.
During treatment, the patient must be provided with abundant drink and a gentle diet.
Treatment of the Coxsackie virus in most cases is carried out at home, hospitalization is necessary only for severe forms of the disease and the development of complications.
Possible complications and consequences
The most frequent complications arising from infection with the Coxsackie virus include pathologies from the central nervous system: cerebral edema, mental disorders, epileptoid seizures, and partial paralysis. In addition, pleurodynia (sharp cramping pain in the intercostal muscles), myopericarditis, heart failure, meningitis, encephalitis, type I diabetes mellitus can become the consequences of the transferred infection.
Forecast
Infectious diseases caused by the Coxsackie virus are usually mild to moderate. The prognosis in the overwhelming majority of cases is favorable, complete recovery occurs within 2-3 weeks. If complications develop, the prognosis worsens. Some complications can be fatal or cause irreversible functional disorders from the affected organs.
Prevention of the Coxsackie virus
General preventive measures aimed at preventing infection with the Coxsackie virus are to control the pollution of sewage waste of the environment, comply with the rules for disinfecting wastewater, and provide the population with food that meets sanitary and epidemiological standards.
There is no specific prophylaxis for the Coxsackie virus.
Individual prevention of viral infection consists in observing the rules of personal hygiene, the necessary processing of products before eating. Disinfection measures should be carried out in foci of infection. During an epidemic, it is recommended to avoid staying in crowded places.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!