- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Knee arthrosis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Knee arthrosis degree
- Knee arthrosis symptoms
- Diagnostics
- Knee arthrosis treatment
- Possible complications and consequences
- Forecast
- Prevention
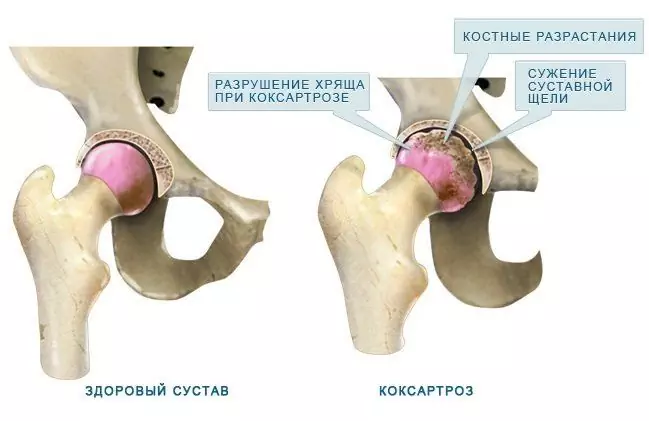
Arthrosis of the knee joint (gonarthrosis) is a chronic degenerative-dystrophic disease of the knee joint, which is characterized by the destruction of articular cartilage, deformation of the knee joint, followed by restriction of movement in it.

Cartilage destruction in arthrosis of the knee joint
Arthrosis of the knee joint ranks first in terms of prevalence in the general structure of arthrosis. The disease affects mainly people over forty years old - in this age group, arthrosis of the knee joint is more common in women, among younger patients, males predominate. In about 6-7% of cases, arthrosis of the knee joint leads to disability.
The knee joint is formed by the articular surfaces of the femur and tibia. The front surface of the knee joint is protected by the patella (patella). The articular surfaces of the femur and tibia, as well as the posterior surface of the patella, are covered with densely elastic hyaline cartilage, the thickness of which is 5-6 mm. Under shock loads, the cartilage performs a shock-absorbing function, and during movement it reduces friction. In clinically healthy people, the processes of synthesis and destruction of cartilaginous tissue are in equilibrium, when the balance is disturbed towards an increase in destruction, arthrosis develops. With arthrosis of the knee joint, blood circulation in the small intraosseous blood vessels that feed the hyaline cartilage is impaired, as a result of which the surface of the cartilage becomes drier, and eventually loses its smoothness. Cracks form on the surface of the hyaline cartilage, which causes regular micro-trauma to the cartilage during movement. With the progression of the pathological process, the cartilage tissue becomes thinner, the articular platform flattens, adapting to the load. Osteophytes appear along the edges of the articular surfaces, which are bony outgrowths formed due to compensatory growth of bone tissue. The pathological process captures the synovial membrane and joint capsule. The joint fluid becomes more viscous, performs its functions worse, which leads to an increase in destructive processes in the joint. With further progression of the disease, the cartilage becomes thinner even more, in some areas it disappears altogether. This leads to a sharp increase in friction between the articular surfaces and deformation of the bones that form the joint. The knee joint is deformed, the deformity can be valgus, i.e. X-shaped, or varus, i.e. O-shaped. Movement in the affected joint is limited until it disappears completely (ankylosis is formed - irreversible and complete destruction of the joint).
Causes and risk factors
The development of arthrosis of the knee joint, as a rule, is caused not by one cause, but by a combination of several factors.
Arthrosis of the knee joint, which occurs in childhood or adolescence, is caused by a violation of the formation of the ligamentous apparatus or articular surfaces. The reason in this case is a genetic predisposition.
Often, gonarthrosis develops against the background of acquired defects of the musculoskeletal system (fractures of the bones of the lower extremities, bruises, dislocations of the knee, ruptures or tears of the ligaments) - it accounts for 20-30% of all arthrosis of the knee joint. The disease usually occurs 3-5 years after the injury, but it can develop as early as several months after the injury. Surgical intervention on the joint can also become the cause of gonarthrosis; in this case, it is a distant complication of the surgical trauma.

Arthrosis of the knee joint is often a distant consequence of trauma: fracture, bruise, dislocation, sprain
Another common reason for the development of arthrosis of the knee joint is overweight, in which the musculoskeletal system, and especially the knee joints, experiences increased stress. In addition, an overweight person is more likely to develop microtrauma or more serious injuries that contribute to the development of arthrosis. An additional risk factor in this group of persons is the presence of pronounced varicose veins of the lower extremities (blood circulation in the legs worsens).
Arthrosis of the knee joint develops with excessive load on the lower limbs, not only in overweight people. The risk group includes athletes, dancers, etc. The greatest danger to the joints of the lower extremities is fast intense squats and jogging. However, a sedentary lifestyle and sedentary work also increase the risk of pathology, since they cause a violation of microcirculation and, accordingly, trophism of the joint.
In addition, arthrosis of the knee joint is formed against the background of such pathological processes as arthritis (reactive arthritis, rheumatoid arthritis, psoriatic arthritis, as well as ankylosing spondylitis), metabolic disorders with subsequent deposition of salts in the articular cavities, innervation disorders in a number of neurological diseases, spinal injuries, craniocerebral trauma.
The onset of arthrosis of the knee joint is facilitated by physiological changes that occur in a woman's body during menopause. During this period, the concentration of estrogens in the blood sharply decreases, which causes the leaching of calcium from the body with the subsequent formation of osteoporosis, manifested by increased fragility of bones and joints.
Some experts believe that a psychological factor (nervous tension, stressful situations) can also contribute to the development of arthrosis of the knee joint.
Forms of the disease
Depending on the etiological factor, the primary (idiopathic) and secondary forms of arthrosis of the knee joint are distinguished. Also, the disease can be unilateral (usually occurs as a result of trauma) and bilateral (develops against the background of overweight, endocrine disorders, in elderly patients).
Knee arthrosis degree
Depending on the severity of pathological manifestations, there are three degrees of arthrosis of the knee joint:
- The cartilage tissue is damaged, but outwardly deformation of the knee joint is not noticeable.
- The cartilaginous tissue is significantly damaged, there is a narrowing of the joint space, bone growth, moderate deformation of the joint can be noticeable on X-rays.
- The cartilaginous tissue becomes thinner, in places exposed areas of the bone are formed, a large number of pathological growths on the surface of the bone tissue are noticeable on X-rays, and pronounced deformation of the joint is noted.

Stages of deformity of the knee joint with arthrosis
Knee arthrosis symptoms
Arthrosis of the knee joint is characterized by gradual development. The severity of the symptoms of arthrosis of the knee joint depends on the degree (stage) of the disease.
The initial period lasting from several months to several years is almost asymptomatic, only from time to time the patient experiences a feeling of discomfort in the knee joint. With arthrosis of the knee joint of the first degree, slight painful sensations appear when moving, especially when going down or climbing stairs. The so-called starting pain is noted, which consists in the appearance of pain during the first steps after lifting from a sitting or horizontal position, it is often accompanied by stiffness of the affected knee joint. There are usually no external changes in the knee, only in rare cases there is a slight edema in the area of the affected joint, which indicates the presence of an inflammatory process in the synovial membrane of the joint. The inflammation leads to the accumulation of fluid in the joint,an increase in its volume, which is accompanied by a feeling of heaviness and restriction of movements.

Knee arthrosis is characterized by pain when walking. The intensity of discomfort depends on the stage of the disease
With arthrosis of the knee joint of the second degree, the pain sensations intensify, the pain accompanies any movement, intensifies with prolonged walking, and is also accompanied by a crunch in the affected joint. Movement in the knee is difficult. At rest, the pain subsides, but with movements it occurs again, often the movements are accompanied by a characteristic crunch. At a given degree of the disease, synovitis appears more often, characterized by a large volume of fluid accumulating in the joint.
For the third degree of gonarthrosis, the presence of pain in the affected knee, even at rest, is characteristic. Soreness can be aggravated when the weather changes, disturb the patient even at night. Usually the pain is localized on the anterior-inner surface of the joint. In the affected joint, movements are sharply limited, both flexion and extension of the leg are disturbed, the patient, as a rule, cannot fully straighten the leg. The affected joint increases in size and is deformed. Due to deformation of the joint and impaired movement in it, the patient develops an unstable waddling gait. In some cases, patients retain the ability to walk only by using a cane, crutches, or walker.
Diagnostics
Anamnesis and an objective examination of the patient are important for the diagnosis. When examining the affected knee joint at the onset of the disease, external changes are not noticeable. At the second and third degree of gonarthrosis, deformation of the knee joint is observed, sometimes the rough contours of the bones that form the joint are visible or palpable, incomplete extension and / or flexion of the leg in the joint, curvature of the tibial axis (usually inward). When flexing and extending the lower limb, a crunch is noted, which, depending on the stage, can be of different severity and duration. A painful area of the knee joint is determined by palpation, usually from the inside of it. With inflammation of the synovial membrane of the knee joint and the accumulation of fluid in it, smoothness of the contours of the joint is observed, with palpation a fluctuation is determined.
To clarify the diagnosis, as well as to determine the degree of arthrosis of the knee joint and differential diagnosis of the disease (including malignant neoplasms), an X-ray examination is performed. When studying X-rays, the fact is taken into account that a number of changes in the knee joint, characteristic of arthrosis of the knee joint, are found in the elderly and in a normal state, that is, they are not necessarily accompanied by pathological manifestations. For this reason, the diagnosis of arthrosis of the knee joint is made in the presence of a combination of characteristic symptoms of the disease with radiological signs of pathology.

The diagnosis of arthrosis of the knee joint is based on clinical cathina in combination with X-ray images
Additional methods of examination for arthrosis of the knee joint are computed tomography (allows you to study in detail changes in bone structures) and magnetic resonance imaging (allows you to determine pathological changes in soft tissues) of the knee joint.
Knee arthrosis treatment
The approach to the treatment of arthrosis of the knee joint of the disease depends on its degree, i.e., the severity of the degenerative process. The goal of therapy is to stop the progression of the disease, eliminate pain, improve joint mobility, and restore (as far as possible) the ligamentous apparatus and destroyed cartilage.
When carrying out conservative treatment of arthrosis of the knee joint, first of all, it is necessary to unload and rest it, otherwise the therapy may not bring the expected effect. For this purpose, if necessary, in a hospital setting, glue or cuff traction is used for the lower leg with small (3-5 kg) loads.
With severe pain syndrome, analgesic drugs are prescribed. As a rule, non-steroidal anti-inflammatory drugs are used for this purpose, especially if it is impossible to apply physiotherapy methods of treatment and massage. It should be borne in mind that, despite the effectiveness, the drugs of this group are not recommended for a long time, since the risk of side effects, mainly damage to the mucous membrane of the gastrointestinal tract, increases. In addition, long-term anesthesia with drugs can hide the appearance of a number of pathological changes and prevent their timely correction. For this reason, non-steroidal anti-inflammatory drugs are prescribed in short courses.
Often, in order to quickly restore the cartilaginous surfaces of the damaged joint, chondroprotectors based on glucosamine and chondroitin sulfate are prescribed. It is believed that combined funds with these components are more effective than monopreparations. These drugs are not recommended for use in patients with increased individual sensitivity to the components of the drug, as well as in patients with phenylketonuria (a genetic disease in which there is a violation of phenylalanine metabolism). In case of arthrosis of the knee joint of the third degree, chondroprotectors are ineffective. It should be noted that, in general, the effectiveness of chondroprotectors has not been confirmed in clinical trials (therapy using these drugs did not show any advantages compared to taking placebo),therefore, many experts do not consider their appointment appropriate.

For arthrosis of the knee joint of 1-2 degrees, chondroprotectors and intra-articular injections of corticosteroid homones are prescribed
For the local symptomatic treatment of arthrosis of the knee joint, preparations are used in the form of a cream, ointment, gel, which have anesthetic and anti-inflammatory effects, as well as improve metabolic processes and blood circulation in the affected knee joint.
In some cases, with arthrosis of the knee joint, intra-articular injections of corticosteroid hormones are used, which have a powerful anti-inflammatory effect. In addition, intra-articular oxygen therapy can be performed, which consists in the introduction of gaseous medical oxygen into the cavity of the knee joint.
After the relief of acute symptoms, the main treatment for arthrosis of the knee joint can be supplemented with physiotherapy: massage of the fascia of the quadriceps muscle of the thigh, mud therapy, ultra-high-frequency therapy, electrophoresis, phonophoresis, magnetotherapy, laser therapy, diadynamic therapy, cryotherapy.
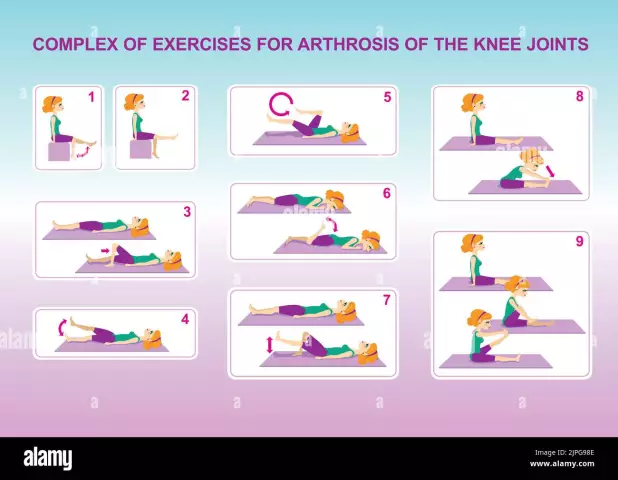
The most effective methods of auxiliary therapy for arthrosis of the knee joint include therapeutic exercises, since it makes it possible to strengthen the muscles, improve blood circulation in the lower limb, and also prevent the occurrence of contractures. Therapeutic gymnastics for arthrosis of the knee joint is carried out exclusively during the period of remission, otherwise it may lead to an aggravation of the pathological process. Exercises for arthrosis of the knee joint are carried out as directed and under the supervision of a physician. When carrying out medical gymnastics, it is important to increase the load gradually, avoiding pain. The first set of exercises is recommended in the morning, before getting out of bed and starting to walk. Usually exercises of therapeutic exercises for arthrosis of the knee joint are recommended to be performed 3-4 times a day,especially when moving from horizontal to vertical position.

Therapeutic gymnastics plays an important role in the treatment of arthrosis of the knee joint
Particular attention is paid to the selection of exercises for arthrosis of the knee joint in women during pregnancy and lactation, since some methods of physiotherapy exercises during this period are contraindicated. Contraindications to therapeutic exercises for arthrosis of the knee joint can be severe diseases of the cardiovascular system, hernia of the anterior abdominal wall, femoral hernia, infectious diseases, especially in the presence of fever.
If there is an inflammatory effusion in the affected knee joint, a puncture is performed. In the case of a chronic course of synovitis, synovectomy is indicated (partial or complete excision of the synovial membrane of the joint capsule). In the presence of highly developed bone growths, they are removed, and if necessary, the free intra-articular bodies are also removed.
In the presence of varus or valgus deformity of the knee joint with severe pain localized on one side of the joint, subcondylar osteotomy of the fibula and tibia is indicated to correct the axis of the lower limb. Corrective osteotomy is aimed at improving the ratio of articular surfaces, as well as normalizing intraosseous circulation, as a result of which venous stasis is eliminated.
In the absence of a positive effect from conservative therapy, especially in case of third-degree arthrosis of the knee joint, a radical operation is indicated - replacement of the destroyed joint with an artificial one (endoprosthetics). After surgery, the patient is rehabilitated, lasting from several months to six months. Modern high-tech endoprostheses are highly reliable and have a long service life - several decades.
For patients with arthrosis of the knee joint, spa treatment is indicated, as well as an individually selected diet.
Possible complications and consequences
Arthrosis of the knee joint can be complicated by atrophy of muscles and ligaments, deformity of the lower limb. The consequence of the disease can be a decrease or complete loss of limb mobility, that is, disability.
Forecast
Provided that arthrosis of the knee joint is diagnosed in the early stages, the cause of the pathological process is eliminated and the prognosis is favorable. The ongoing therapy makes it possible to achieve long-term remission, but the treatment is usually lifelong. In the absence of the necessary treatment, as well as if the patient does not follow the doctor's instructions, arthrosis of the knee joint becomes the cause of disability.
Prevention
In order to prevent the development of arthrosis of the knee joint, as well as to prevent the development of complications with the existing disease, it is recommended:
- timely treatment of pathologies that can contribute to the development of arthrosis of the knee joint;
- balanced diet;
- correction of excess weight;
- sufficient physical activity;
- avoiding heavy lifting and activities associated with intense monotonous movements in the knee joints;
- selection of quality footwear with elastic sole with shock absorption effect.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!