- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Arteriovenous fistula
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Arteriovenous fistula (shunt, fistula) is a direct connection between an artery and a vein, without the participation of the capillary network. This is one of the forms of arteriovenous malformation.
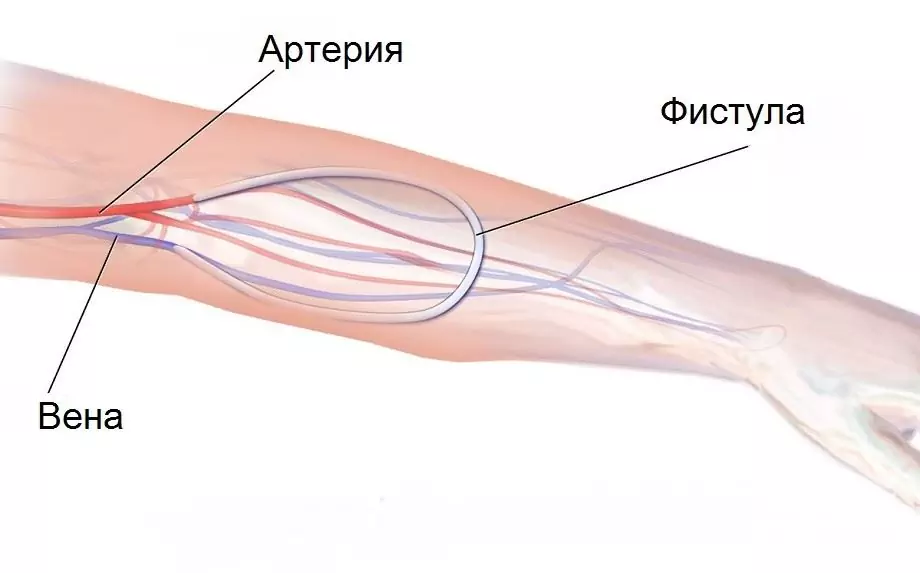
Schematic representation of an arteriovenous fistula
Causes and risk factors
Congenital arteriovenous fistulas are one of the rare congenital malformations. It can be caused by various negative factors that affect the development of the fetus:
- viral infections (flu, rubella, measles);
- bad habits of a pregnant woman (smoking, drug or alcohol use);
- exposure to radiation;
- living in an area with poor environmental conditions;
- taking medications with a teratogenic effect.
Acquired arteriovenous fistulas result from traumatic injury to contiguous veins and arteries. This can lead to not only bullet or stab wounds, but also damage to blood vessels during surgery or puncture biopsy. The formation of a traumatic arteriovenous fistula occurs very quickly, literally within 2-5 hours.
In some cases, surgeons create an arteriovenous fistula on purpose. Such an anastomosis between a vein and an artery is necessary for hemodialysis: it prevents repeated punctures of large blood vessels. Most often, an artificial fistula is applied between the vessels of the forearm.

Arteriovenous fistula for hemodialysis
Forms of the disease
Arteriovenous fistulas are divided into congenital and acquired, depending on the cause and timing of their occurrence. The latter, in turn, are subdivided into traumatic and artificial.
Depending on the place of localization, the following forms of pathology are distinguished:
- dural fistulas (in the dura mater);
- spinal fistulas (in the spinal cord);
- pulmonary fistulas (between the pulmonary vein and the aorta);
- abdominal fistulas;
- fistulas of the subclavian artery;
- fistulas of the lower or upper extremities.
Arteriovenous fistulas can also be:
- Straight (artery and vein adjacent directly to each other).
- Indirect (the artery and veins that form the fistula are connected through the aneurysmal sac).
Depending on the prevalence of the pathological process, there are:
- Generalized form (multiple fistulas leading to disruption of the blood supply to the large segment).
- Localized form (one shunt between a vein and an artery, often combined with other malformations).
Symptoms
Small fistulas are usually asymptomatic, manifesting clinically only with an increase in size. In this case, there are:
- redness and swelling of the skin;
- well visible swollen veins;
- swelling of the limbs;
- lowering blood pressure;
- weakness, decreased performance.

Bloated veins from arteriovenous fistula
With large fistulas, a significant decrease in blood pressure is observed, which causes an increase in heart rate. This leads to the formation of heart failure, which is characterized by:
- cyanosis of the skin;
- feeling short of breath;
- dyspnea;
- deformation of the fingers like drumsticks (thickening of the terminal phalanges).
Diagnostics
Diagnosis of arteriovenous fistulas begins with the study of the family history and patient complaints, his examination. On auscultation, a characteristic vascular murmur can be heard in the area above the fistula.
To confirm the presence of an arteriovenous fistula and assess its size, instrumental diagnostics are performed:
- angiography;
- ultrasound dopplerography;
- CT angiography.
Treatment
The choice of treatment method for arteriovenous fistulas depends on their location, size, duration of the disease, the general condition of the patient, the presence or absence of concomitant pathology.
The most effective is open surgical removal of the fistula, that is, traditional surgery with an incision in the skin.

For small arteriovenous fistulas, laser coagulation is possible
If catheterization of the fistula is possible, endovascular surgery may be performed. It consists in the following: an artery is punctured, a catheter is inserted through a needle into it, which is advanced to the anastomosis between the artery and the vein. Then a special drug (sclerosant) is injected through the catheter, causing the fistula walls to stick together.
Small arteriovenous fistulas can be removed with radiosurgery or laser coagulation.
Possible complications and consequences
In the absence of treatment and significant sizes of arteriovenous fistulas, the following complications can occur:
- chronic heart failure;
- thrombosis;
- formation at the site of the shunt aneurysm;
- ischemic strokes;
- pulmonary embolism.
Forecast
With timely removal of the arteriovenous fistula, the prognosis is favorable. With the addition of complications, it worsens.
Prevention
Prevention of the development of congenital arteriovenous fistulas is impossible. To prevent the formation of acquired fistulas, timely and adequate treatment of injuries, careful hemostasis during surgical interventions are required.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!






