- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Parathyroid hormone is elevated - what does it mean?
The content of the article:
-
What does an increase in parathyroid hormone in the blood mean?
- Primary hyperparathyroidism
- Secondary hyperparathyroidism
- Tertiary hyperparathyroidism
-
Symptoms
- Bone damage
- Kidney pathology
- Lesion of the gastrointestinal tract
- Other symptoms
- Diagnostic methods
-
Treatment
- Surgery
- Conservative treatment
-
What is parathyroid hormone?
- Where is it produced
- How does
- Video
If the parathyroid hormone is elevated - what does it mean? Parathyroid hormone reflects the work of the parathyroid glands. It regulates the exchange of calcium and phosphorus in the human body. The deviation of its content in the blood from the norm signals the presence of any disease. An increase in the indicator can be observed with insufficient calcium intake, pathology of the parathyroid glands, kidneys, and intestines. As a result, calcium-phosphorus homeostasis is disturbed, which affects the whole body.

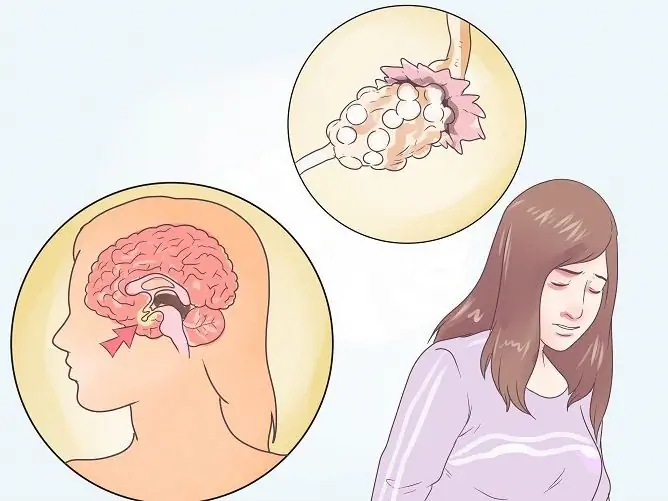
Parathyroid hormone regulates phosphorus-calcium metabolism, its increase affects primarily the bones and kidneys
What does an increase in parathyroid hormone in the blood mean?
An increase in parathyroid hormone in the blood indicates hyperparathyroidism. Women get it more often than men. The disease can develop at any age, but more often in people over 50. The high incidence rate in women is observed during the postmenopausal period.
Most often, this condition is associated with damage to the parathyroid glands. Less commonly, PTH synthesis increases compensatory in response to hypocalcemia. Depending on the cause, there are three types of hyperparathyroidism - primary, secondary and tertiary.
Primary hyperparathyroidism
In primary hyperparathyroidism, excess PTH secretion is associated with damage to the parathyroid glands. The following conditions can be the cause of the development of the disease:
- benign formations - solitary or multiple adenoma;
- malignant neoplasms - carcinoma;
- hyperplasia of the glands.
In most cases, excessive secretion of parathyroid hormone is caused by solitary adenoma, other pathologies are less common.
Secondary hyperparathyroidism
In secondary hyperparathyroidism, the functioning of the parathyroid glands is not impaired. Pathology occurs secondarily as a compensatory response to hypocalcemia. In response to a prolonged decrease in blood calcium, there is an increase in the production of parathyroid hormone.
A decrease in the level of calcium in the blood can be for the following reasons:
- alimentary - insufficient intake of calcium from food;
- excess vitamin D;
- violation of calcium absorption - pathology of the small intestine;
- renal failure.
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism is less common than other forms. The disease is characterized by the development of adenoma against the background of long-term existence of secondary hyperparathyroidism.
Symptoms
Hyperparathyroidism is accompanied by damage to the musculoskeletal system, kidneys, and gastrointestinal tract. Additionally, changes in the heart and nervous system may occur, but these symptoms are not specific to hyperparathyroidism.
Bone damage
Parathyrin activates the leaching of calcium from bone tissue. This leads to a decrease in bone density. They become more fragile, which is often accompanied by fractures.
Symptoms of damage to the musculoskeletal system:
- chronic bone pain;
- pathological fractures of the ribs, pelvis, lower extremities;
- deformation of the skeleton;
- gait disturbances;
- overgrowth of bone tissue.
Kidney pathology
Excess calcium leads to damage to the excretory system. When a large amount of calcium is excreted in the urinary tract, stones are formed - urolithiasis develops.
The main clinical manifestation of urolithiasis is renal colic. Pain occurs due to obstruction of the urinary tract and has the following characteristics:
- occurs paroxysm;
- has a spastic character;
- gives to the thigh, external genitals;
- localized in the lumbar region.
In severe cases, the excretory and filtration function of the kidneys is impaired, which leads to the development of renal failure.
Lesion of the gastrointestinal tract
Hypercalcemia leads to the development of degenerative processes in the gastrointestinal tract. This is manifested by the following symptoms:
- nausea, vomiting;
- abdominal pain;
- a tendency to constipation;
- weight loss.
Ulcers of the stomach and duodenum are often detected. In addition, an excess of parathyroid hormone can lead to the formation of calcifications in the pancreas.
Other symptoms
Less commonly, hyperparathyroidism develops damage to the heart and nervous system. Damage to the cardiovascular system can manifest itself in the following symptoms:
- blood pressure rises;
- there are interruptions in the work of the heart (arrhythmias);
- with physical exertion, shortness of breath and pain in the chest region appear.
Disruption of calcium metabolism can provoke the appearance of neuropsychiatric disorders. These include:
- general weakness;
- increased fatigue;
- drowsiness;
- convulsions;
- paresthesia (numbness, tingling in the limbs);
- impairment of cognitive functions.
These symptoms are not specific, therefore, they can indicate not only hyperparathyroidism, but also other diseases.
Diagnostic methods
An increased level of parathyroid hormone is determined by a blood test. What numbers indicate hyperparathyroidism:
- Up to 22 years - above 95 pg / mol.
- At the age of 23-70 years - above 75 pg / mol.
- Over 70 years - over 117 pg / mol.
If hyperparathyroidism is detected, additional examination is necessary. This is necessary to determine the form of the disease and the selection of therapy.
| Study | Description |
| Blood calcium level | In most cases, blood calcium levels are elevated (hypercalcemia), but normal calcium levels are possible. In this case, the level of vitamin D and creatinine is necessarily examined. |
| Biochemical blood test (creatinine) | To assess the condition of the kidneys, creatinine levels are examined and the glomerular filtration rate (GFR) is calculated. |
| Ultrasound of the parathyroid glands | With ultrasound, the size and structure of the parathyroid glands can be assessed. The main advantages of the method are availability and low cost. However, due to the low information content, additional computed tomography is often required. |
| CT scan | For a more specific study, computed tomography (CT) is prescribed with intravenous administration of contrast agents. With the help of CT, it is possible to determine even atypical localization of the glands, to visualize tumor formations. |
In hyperparathyroidism, mainly bone tissue and kidneys are affected. To assess their condition, as well as the condition of the digestive tract, the following studies can be used:
- X-ray of bones. It is carried out to diagnose pathological fractures, osteodystrophy and other bone disorders. An X-ray examination of the hands, pelvis, and tubular bones can be performed.
- Ultrasound of the kidneys. The study reveals kidney damage in the form of nephrolithiasis (single or multiple stones).
- Fibrogastroduodenoscopy (FGDS). The study is prescribed with pronounced signs of damage to the gastrointestinal tract. With the help of EGDS, it is possible to identify erosion and ulcers in the stomach and duodenum.
These studies are not used to confirm the diagnosis, but only to assess the degree of damage to target organs.
Treatment
Treatment for an increase in parathyroid hormone in the blood can be conservative or surgical. Surgical is the most effective, therefore it is indicated for those patients who have clinical manifestations of the disease. If a laboratory increase in parathyroid hormone in the blood is not accompanied by any symptoms, conservative therapy is possible.
Surgery
Surgical intervention is the most radical and effective method. The operation is performed under general anesthesia. Removal of both all and only one parathyroid gland is possible.
The least traumatic and dangerous is selective parathyroidectomy. During this operation, a minimal incision is made, then the affected parathyroid gland is removed. The rest of the glands are not injured.
Conservative treatment
There is no equal equivalent to surgical treatment, since no drug can achieve the same normalization of the function of the parathyroid glands. Conservative treatment is indicated in cases where hyperparathyroidism is not accompanied by pathological changes in the internal organs. For conservative treatment, the following medicines are used:
- Thiazide diuretics - Hydrochlorothiazide. The drug increases the reabsorption of calcium in the kidneys.
- Antiresorptive drugs - bisphosphonates, Denosumab. They inhibit the processes of bone resorption (resorption of bone tissue), which leads to a decrease in the calcium content in the blood.
- Cinacalcet. The drug reduces the concentration of parathyroid hormone in the blood.
Also, drug therapy is carried out in the presence of contraindications to surgery, relapse after surgery.
In addition to medications, it is recommended to follow a diet with limited calcium intake (up to 1000 mg / day), increase fluid intake.
What is parathyroid hormone?
Parathyroid hormone (PTH, parathyrin) is a hormone that regulates the level of calcium and phosphorus in the body. Normal calcium levels are maintained through the effects of parathyrin on bone tissue, kidneys and intestines.

Parathyroid hormone is produced in the parathyroid glands
Where is it produced
In the parathyroid glands, a preparathyroid hormone is produced, which breaks down to form the proparathyroid hormone. It, in turn, is converted to biologically active parathyroid hormone.
How does
The main function of PTH is to regulate calcium-phosphorus metabolism. The hormone increases the calcium content in the blood by acting on target organs:
- bones;
- kidneys;
- intestines.
In bones, PTH activates osteoclasts and osteoblasts, specific cells of bone tissue. Under the action of parathyroid hormone, bone tissue is resorbed by dissolving the mineral component. At this stage, a large amount of calcium enters the bloodstream. Then the osteoblasts - cells that create new bone tissue - are activated.
In the kidneys, PTH increases the reabsorption of calcium, that is, its reabsorption into the body. As a result, less calcium is excreted in the urine, so the content of the trace element in the blood rises. The effect on phosphate metabolism is the opposite - parathyroid hormone increases their excretion in the urine.
In the intestine, PTH stimulates the conversion of vitamin D, which increases intestinal absorption of calcium.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.