- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Menstruation after miscarriage
For every woman who has experienced a miscarriage, the most important thing is to get out of this situation with the minimum possible losses - to give birth after this healthy baby.

The next pregnancy after a miscarriage is planned, and normal periods after a miscarriage are an integral part of a woman's health and future conception.
What you need to know about your period after a miscarriage
Bleeding is an integral companion and the first symptom of a miscarriage. Strictly speaking, the first day of bleeding that accompanies a spontaneous abortion is considered the first day of menstruation after a miscarriage. On average, such menstrual bleeding lasts about ten days. Over the next month and a half, minor bleeding may recur periodically. Their duration and intensity are directly influenced by factors such as the transferred nervous stress, the presence of concomitant infections or bacterial complications.
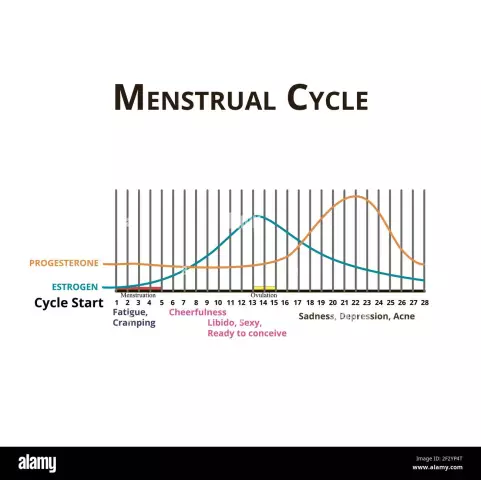
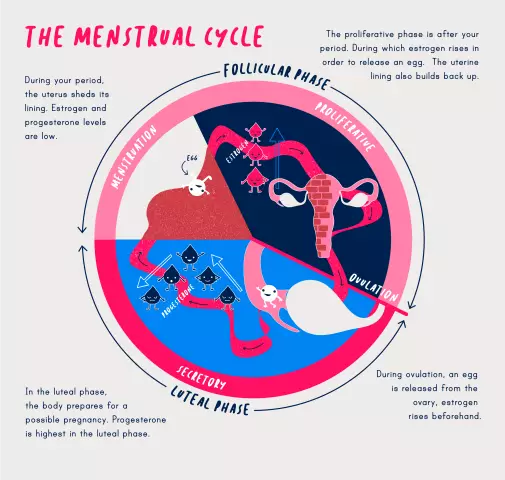
A full next period after a miscarriage should normally begin in 21-35 days. It should be borne in mind that in the overwhelming majority of cases, miscarriage is a cause or a consequence of hormonal imbalance in a woman's body, therefore, the first few cycles after a miscarriage may be longer than usual. Since the regularity of menstruation after a miscarriage is restored within a certain period of time, a woman should consult a gynecologist about her desire to use oral contraceptives.
The first menstruation after a miscarriage is often profuse. Over the next few months (usually no more than two), the volume of menstrual bleeding should normalize, otherwise there is reason to assume the presence of other diseases of the pelvic organs or an infection. Such a complication is dangerous by the possibility of the development of profuse uterine bleeding, which threatens the life of a woman, requires hospitalization and adequate medical measures in a hospital setting.
Massive periods after a miscarriage often lead to the development of iron deficiency anemia. Symptoms of the disease are increased fatigue, weakness, drowsiness, pallor of the skin. When confirming the diagnosis, the doctor prescribes to the patient iron-containing drugs in an individual dosage, in order to normalize her condition.
Modern medicine differentiates miscarriages on a number of grounds. So, they distinguish:
- Threatened miscarriage;
- Failed miscarriage;
- Incipient miscarriage;
- Incomplete miscarriage.
If, after a miscarriage, severe bleeding occurs, regardless of the type, a decision is made on additional curettage of the uterine cavity and subsequent ultrasound control of its quality. This procedure has a direct impact on the nature of menstruation after a miscarriage. If the remains of fetal tissue remain in the uterine cavity after a miscarriage, this can lead to infection, bacterial and inflammatory complications, the development of profuse menstruation after a miscarriage and even bleeding.
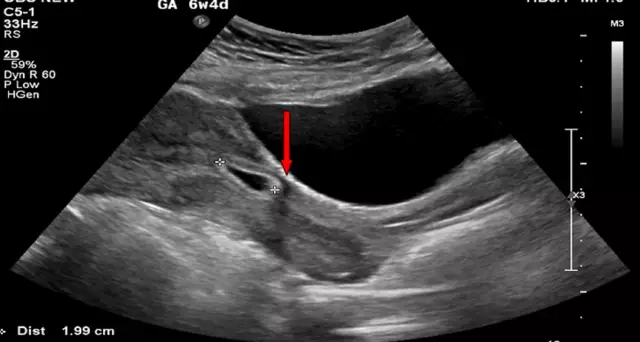
If there is no profuse bleeding, then in modern gynecology it is customary to limit itself to ultrasound monitoring of the state of the uterine cavity after a miscarriage approximately once every seven days. In a situation where the uterus is clean or has a small number of clots, but the woman's condition is satisfactory, drug treatment is indicated - antiprogestins, prostaglandins, etc., as well as medical control using ultrasound.
According to statistics, more than 70% of miscarriages end in self-cleaning of the uterus after a miscarriage. Expectant tactics, if indicated, lasts from two to four weeks.
Post-miscarriage cycle
Curettage helps to avoid these and other negative consequences of spontaneous abortion, and fetal tissues sent for histological examination make it possible to establish the cause of the miscarriage and prescribe an adequate medical correction of the condition. In general, such a complex of measures allows planning the next pregnancy with minimal risks to the health of the mother and fetus.
In order to normalize the cycle after a miscarriage, a course of treatment is also prescribed. Typically, it consists of:
- Anti-inflammatory;
- Antibacterial;
- Antifungal;
- Iron-containing;
- Hemostatic drugs;
- Medicines that cause uterine contractions.
The restoration of sexual relations is shown after one menstrual cycle, since the tissues of the uterus after a miscarriage are still traumatized and can be infected during sexual intercourse; the first sexual contacts should be protected.
You need to know that a pregnancy that occurs soon after a miscarriage has a high probability of the same unfavorable outcome, therefore, together with a doctor, it is necessary to choose a method of contraception that is suitable from different points of view (as a rule, these are oral contraceptives).
The female body needs to recover, to establish the cause of the miscarriage, including examinations of the hemostasis system, and full treatment. It is correct to plan for conception only five to six cycles after a miscarriage (at least three). Before that, it is important to make sure that the menstrual cycle is regular, as well as adhere to a healthy lifestyle - normalize diet and sleep, introduce regular physical activity and walk in the fresh air. A woman needs to give up bad habits and maintain an adequate emotional state.

All of the above applies to planned pregnancy. If conception soon after a miscarriage nevertheless happened unplanned, then you should not despair - it is likely that the body is already ready for a new pregnancy. You should only immediately notify your doctor about it and follow all his recommendations.
Uterus after miscarriage
No less dangerous than heavy periods after a miscarriage, for a woman, menstruation is scarce. After the spontaneous termination of pregnancy itself, as well as in response to the subsequent curettage, synechiae, that is, adhesions, may form in the uterus after a miscarriage. Intrauterine synechiae have a spiral-like effect, that is, they act as a local mechanical contraceptive and prevent conception.
Also, scanty periods after a miscarriage can indicate hormonal disorders caused by stress. For reliable diagnosis, the patient is prescribed laboratory tests on the 2-3rd day of the menstrual cycle, and hysteroscopy is also performed. In addition, the patency of the fallopian tubes is examined using hysterosalpingography or sonohysterosalpingography.
YouTube video related to the article:
Found a mistake in the text? Select it and press Ctrl + Enter.