- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Intracranial pressure: symptoms in adults, causes, diagnosis, treatment
The content of the article:
- What is intracranial pressure?
- What causes increased intracranial pressure
- Signs of intracranial hypertension
- Diagnostics
- How to treat intracranial hypertension
- Video
Intracranial pressure can normally range from 7.5 to 15 mm Hg. Art. In children, normal values are slightly lower than in adults. An increase in values above normal (intracranial hypertension), as a rule, is of a secondary nature and is a pathological condition that can occur in adults and children and lead to the development of adverse consequences. At values over 30 mm Hg. Art. possibly irreversible damage to brain tissue, including leading to death.
What is intracranial pressure?
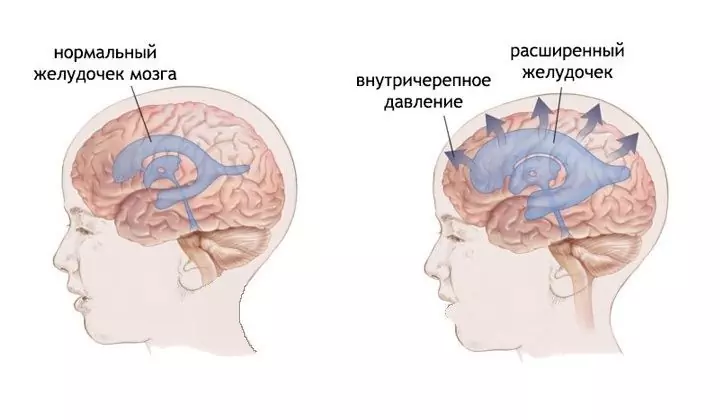
The pressure inside the skull is primarily due to the pressure of the cerebrospinal fluid (CSF) contained in some structures of the brain, partly by the pressure of blood in the vessels, and in some cases - tissue fluid.
Why is raising it dangerous? The fact is that the brain is located in the cranium, that is, it is rigidly limited by bone structures. An increase in pressure in such a confined space leads to compression of the brain structures, which causes neurological disorders, primarily headache. Long-term intracranial hypertension can cause severe complications.

Increased cranial pressure is manifested primarily by intense headache
The pressure inside the skull, in contrast to the arterial pressure, cannot be measured at home independently; for this, special instrumental methods are used. How do you know if a person has high cranial pressure? Usually, its presence is indicated by a characteristic triad of signs:
- Headache.
- Vomiting.
- Congestive fundus (determined by an ophthalmologist).
What causes increased intracranial pressure
Usually, intracranial hypertension occurs with an increase in the volume of cerebrospinal fluid, tissue fluid (cerebral edema), blood (venous congestion), as well as when neoplasms (cyst, tumor, hematoma) form in the brain.
A short-term increase in cranial pressure occurs in healthy people when coughing, sneezing, tilting the body, stressful situations, excessive physical exertion, etc. However, in such cases, it quickly returns to normal.
A prolonged increase in pressure inside the skull, as a rule, is a clinical sign of a particular disease, and is not an independent pathology, that is, it is of a secondary nature. The reason for the persistent increase in intracranial pressure is craniocerebral trauma, inflammation of the brain and its membranes (meningitis, encephalitis), neoplasms in the head area, stroke, hydrocephalus. Less commonly, intoxication with heavy metal salts, poisonous gases, methyl or ethyl alcohol.

Intracranial hypertension can be caused by a neoplasm in the brain
The development of intracranial hypertension is a genetic predisposition, overweight, hypertension, hyperthyroidism, adrenal and / or liver disorders, parasitic diseases, osteochondrosis of the cervical spine, otitis media, bronchitis, mastoiditis, taking certain medications (antibacterial drugs, corticosteroids, oral contraceptives).
In infants, the causes of the pathological condition can be late toxicosis in the mother during pregnancy (gestosis), prenatal hypoxia, birth trauma (the main cause of pathology in children of the first year of life), and prematurity.
A pathological decrease in pressure inside the skull (intracranial hypotension) can occur against a background of violation of the integrity of the bones of the skull and meninges, overdose of certain drugs, loss of cerebrospinal fluid during lumbar puncture or drainage of the ventricles of the brain.
Signs of intracranial hypertension
The main symptom of intracranial pressure in adults is headache, vomiting, and fundus congestion.
Pain syndrome with increased cranial pressure has a certain character: the headache intensifies in the morning, which is explained by the increased production of cerebrospinal fluid from 4 to 6 in the morning; or after waking up at another time (for example, after a nap). Bursting pain, pressing on the eyes. It increases with coughing and sneezing, as well as with a change in body position, especially when lowering the head. Taking analgesics does not bring relief.
Vomiting in this case is not associated with food intake. It also appears frequently in the morning and may be multiple. After it, the intensity of the headache decreases.
The so-called stagnant optic nerve head, or fundus stagnation, is swelling of the optic nerve head, found during ophthalmologic examination. This is one of the pathognomonic, that is, characteristic of this particular condition, signs. The rest of the symptoms of intracranial pressure in women and men are not specific and can be observed in other diseases.
Other symptoms: dizziness, visual disturbances, drowsiness, lethargy, fatigue, distraction, memory impairment, irritability, mood swings, increased or decreased blood pressure. Also, patients may complain of increased salivation, nausea, increased sweating, chills, increased skin sensitivity, shortness of breath, muscle paresis, pain in the spine.
Disturbances on the part of the visual analyzer are common symptoms, which include decreased peripheral vision, double vision, blurred vision, periodic attacks of blindness, and decreased response to light. In addition, the shape of the eyeball may change in patients. In some cases, the eyeball protrudes so much that the patient is unable to completely close his eyes.

Vomiting, after which the headache decreases, is one of the symptoms of intracranial hypertension
It is much more difficult to understand that cranial pressure is increased in babies. This condition is manifested by lethargy, tearfulness, swelling of the fontanelle and its pulsation, enlargement of the head, protruding of the network of blood vessels on the scalp, seizures, involuntary eye movements. In infants, vomiting, uneven muscle tone (some muscles are relaxed and some are tense), sleep disturbances may occur.
Pathology tends to progress and, in the absence of timely adequate treatment, can lead to the development of consequences, including irreversible ones, associated with prolonged compression of the brain structures. These include: impaired coordination of movements (with damage to the cerebellum), cardiac arrhythmias, reflexes (in the case of compression of the brain stem), speech disorders, mental disorders, loss of vision, paralysis, stroke, epilepsy, death.
The risk of death increases if the patient has gait disturbances, urinary and fecal incontinence, disorders of the cardiovascular and respiratory systems, loss of consciousness, coma.
Diagnostics
To make a diagnosis, the data obtained during the collection of complaints and anamnesis, examination of the patient, in particular, ophthalmic, are used. Examination of the fundus makes it possible to detect characteristic small hemorrhages on the retina, an increase in the blood vessels of the eyeball, and edema of the optic nerve head. The detection of such signs in the presence of a characteristic clinical picture makes it possible to establish an increased cranial pressure.
To detect a primary disease, an examination is carried out, which includes laboratory and instrumental methods (computed or magnetic resonance imaging, electroencephalography, etc.).

Fundus examination reveals characteristic optic disc edema
The choice of one or another method for measuring the pressure inside the skull depends on the age of the patient and the characteristics of the course of the disease. In children of the first year of life, neurosonography and echoencephalography are usually used. A puncture of the ventricles of the brain (or lumbar spine) with pressure measurement may be necessary. Puncture performs another role - it allows laboratory diagnostics of cerebrospinal fluid in case of suspicion of an infectious or neoplastic nature of the pathology. When measuring, cyclical changes in the indicator should also be taken into account, which allows you to obtain more information than when determining a separate average value.
During the diagnosis, edema, an increase or decrease in the volume of the ventricles of the brain, hemorrhages, neoplasms, an increase in the space between the meninges, divergence of the cranial sutures, displacement of brain structures and other changes in the structure of the brain and surrounding tissues can be detected.
Differential diagnosis is carried out with epilepsy, migraine, metabolic diseases, psychosomatic disorders (psychosomatics in medicine - the development of somatic, i.e., bodily diseases under the influence of psychological factors).
How to treat intracranial hypertension
What to do if cranial pressure rises? How to get rid of it? Treatment goes in two main directions:
- Reduction of intracranial pressure in order to eliminate the compression of brain structures and painful symptoms of pathology.
- Elimination of the cause of intracranial hypertension, i.e. treatment of the underlying disease.
Depending on the results of the examination, both conservative and surgical methods can be used.
The primary goal of conservative, and in difficult cases and surgical treatment is to reduce the pressure of the cerebrospinal fluid.
Drug therapy consists in the appointment of diuretics - diuretics that allow you to remove excess fluid from the body and thereby reduce pressure, including intracranial pressure. Also used are drugs that improve cerebral circulation, steroid anti-inflammatory drugs, pain relievers and antiemetics.

Neck massage can help relieve mildly increased cranial pressure
In some cases, physiotherapy is used: magnetotherapy, electrophoresis of drugs, acupuncture, massage of the spine and cervical-collar zone, physiotherapy exercises, circular shower. Such methods are usually used in uncomplicated forms of pathology, when there is no danger to the patient's life.
In addition to the main treatment, remedies based on medicinal plants (tincture of peony, peppermint, motherwort, valerian) can be used.
Surgical treatment is resorted to in case of ineffectiveness of drug therapy or for health reasons. It consists in bypassing, creating an artificial pathway for the outflow of cerebrospinal fluid. Excess cerebrospinal fluid through a specially inserted tube will be pumped from the ventricles of the brain into the abdominal cavity or into the space between the meninges at the base of the brain. If a shunt is being placed in a child, it may be necessary to lengthen it several times as the child grows.
In addition, surgical treatment is carried out in the treatment of certain neoplasms - aneurysms, hematomas, cysts, tumors.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.