- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Intracranial pressure in children: symptoms, causes, treatment
The content of the article:
- Symptoms of intracranial pressure in children
- Causes of increased intracranial pressure
- How to determine intracranial pressure in children
- Treatment of intracranial pressure in children
- Video
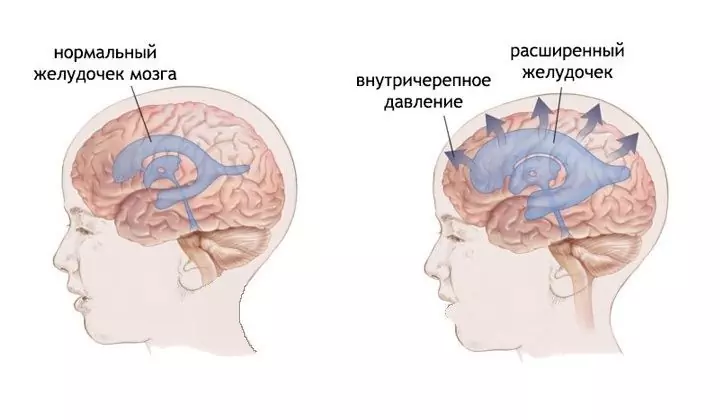
What is intracranial pressure in children, and are there any differences from adults? The structure of the human skull assumes the presence of a closed system of channels containing cerebral fluid - cerebrospinal fluid. It constantly circulates, performing a number of tasks - from trophism (nutrition) of the brain to protecting it from injury and concussion. CSF can exert pressure on the structures of the brain; it is this parameter that is called intracranial pressure. Children are especially sensitive to changes in intracranial pressure due to the special vulnerability of the nervous system due to age, as well as the presence of cartilaginous structures in the skull.

Increased intracranial pressure in young children may manifest as an enlarged head
Symptoms of intracranial pressure in children
Signs of intracranial pressure in a child vary depending on the age and nature of the pathology. Several age groups are distinguished to differentiate the clinical picture - children from 2 years to 5 years old are referred to the younger group, and from 5 to 9 years old - to the older one. Due to ossification of the skull structures, intracranial pressure lends itself well to conservative treatment in older children (10 and 11 years old) - that is why it is not critically dangerous for them.
Symptoms common in young children include:
- Restlessness in the evening and at night, sleep disturbances, crying violently. The cause is an increase in intracranial pressure due to the horizontal position of the body. In this case, the venous system of the skull receives more blood, so the sinuses swell and the pressure rises.
- Nausea and vomiting. Associated with pressure on the structures of the medulla oblongata, which are responsible for the gag reflex. It is necessary to distinguish this symptom from vomiting associated with overfeeding of the child or food poisoning. Vomiting of central genesis is not associated with food intake, occurs several times a day, and the nature of the vomit does not change.
- Increased head size. This is possible in a baby under 1 year old, as in older children the fontanelles ossify. In young children, the cartilaginous structures in the skull dominate, so the fontanelles swell, the seams of the skull diverge, and the frontal lobe increases significantly. Visually, this is manifested by an increase in the head.
- Marked subcutaneous venous network. E If the child increased cranial pressure, and congested veins contrasted under the skin as well noticeable vasculature.
- Graefe symptom. This symptom is specific for birth trauma, but sometimes it also manifests itself with an increase in pressure in the CSF system. It is characterized by spontaneous downward movements of the eyes, with a white stripe of sclera visible between the upper edge of the iris and the upper eyelid.
Nonspecific symptoms associated with an increase in intracranial pressure indirectly - frequent crying, refusal to feed, developmental delay, lethargy and lethargy.
Older children may complain about the subjective sensations that high blood pressure causes them. In this case, it is somewhat easier to diagnose the pathological condition. Main features:
- Vomiting that does not bring relief. It occurs due to irritation of the vomiting centers. Repeated many times, the child complains of nausea, which does not go away after an attack of vomiting.
- Headache. Soreness is felt behind the eyeballs (the cerebrospinal fluid presses on the space behind them), as well as in the area of the frontal and temporal lobes.
- Symptoms of irritation of the optic nerves. The child complains of flashes in front of his eyes, colored "trains" that reach for objects, double vision.
- Sleep disturbances. Caused by increased compression of the brain and soreness in the supine position.
High intracranial pressure deprives the child of appetite, makes him lethargic and moody throughout the day.
A further increase in intracranial pressure can lead to the development of dangerous consequences. On the part of the nervous system, this is mental retardation (especially dangerous during the active formation and development of the brain - at 3-4 years old), lag in physical development, visual impairment and other neurological disorders.
Causes of increased intracranial pressure
What causes an increase in pressure inside the skull? All causes of high cerebral fluid pressure are divided into organic and functional. The former suggest the presence of organic pathology, and the latter - a violation of the function of the cerebrospinal fluid circulation. It is necessary to understand that there is no direct evidence, except for measuring pressure, and its optimal indicators are individual for each, there are only average age standards.
Organic reasons include:
- brain injury with subsequent deformation of brain structures;
- infectious diseases of the brain: encephalitis, meningitis;
- brain tumors;
- toxic damage to brain tissue;
- intracerebral hemorrhage.
Functional reasons include:
- a large amount of cerebrospinal fluid in the ventricles of the brain;
- poor circulation conditions of cerebrospinal fluid - deterioration of its outflow or passage through the appropriate channels;
- vegetative-vascular dystonia, violation of muscle tone.
Intracranial pressure can fluctuate under the influence of atmospheric pressure, so a slight increase in it does not necessarily indicate any pathology.
How to determine intracranial pressure in children
It will not be possible to independently establish a diagnosis and find out the exact value of intracranial pressure - for this you need to contact a neurologist. He will collect anamnesis, ask parents about the primary manifestations, and also examine the child and determine which of the symptoms are most pronounced. The doctor pays special attention to pathological reflexes of the eyeball, bulging fontanelles. To understand whether the condition is independent or caused by another disease, it is necessary to measure the pressure of the cerebrospinal fluid and compare it with the age norm.

If you suspect increased intracranial pressure, the child should be examined by an ophthalmologist
When a neurologist identifies characteristic signs, the patient is sent for a consultation with an ophthalmologist. The ophthalmologist will check vision (long-term increased intracranial pressure causes its deterioration), examines the fundus, where angiopathies can be found, which indicate a persistent and long-term increase in pressure in the skull.
What to do next? The next step in diagnosis is neurosonography, or ultrasound of the brain. This method is most informative in young children with soft areas of the skull. Neurosonography allows you to see the deformation of the midline structures of the brain, changes in the size and position of the ventricles of the brain, the displacement of the median interhemispheric fissure. This method is non-invasive and harmless to the child, if you observe the frequency of the examination. In children 6, 7 and 8 years old, when the fontanelles are already completely overgrown, CT (computed tomography) and MRI (magnetic resonance imaging) of the brain are performed.
If the diagnosis of increased intracranial pressure is confirmed and has a morphological substrate, treatment is prescribed.
Treatment of intracranial pressure in children
How to relieve high intracranial pressure? For this, a complex therapy is prescribed, aimed at reducing clinical manifestations and removing the primary cause of the pathology. At the same time, preventive measures are taken that significantly increase the effectiveness of treatment - they normalize sleep and wakefulness, ensure the child's daily stay in the fresh air, balanced nutrition, moderate but regular physical activity (in particular, swimming).
Drug therapy consists in the use of diuretics that remove moisture from the body, reduce the volume of circulating blood and, accordingly, the amount of cerebrospinal fluid formed in the ventricles of the brain, thereby helping to relieve edema with accompanying pain. Also, nootropics and other drugs are prescribed to normalize cerebral circulation - these funds compensate for blood stagnation, improve cerebral circulation.
Additionally, a wide spectrum of cerebroprotectors can be used - they affect the brain tissue, the endothelium of the vessels feeding the brain, normalize the electrolyte balance after the use of diuretics, and improve the conductivity of brain impulses. Painkillers and sedatives (sedatives) are also used to relieve unpleasant symptoms and improve nighttime sleep.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.