- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Intestinal infarction - what is it?
The content of the article:
- The mechanism of development of the disease
- Causes and risk factors
- Classification
- Disease stages
- Bowel infarction symptoms
- Diagnostics
- Treatment
- Video
Intestinal infarction is a disease in which there is a blockage of the bloodstream of the mesentery, and then, due to an acute disturbance of blood supply, necrosis of the intestinal wall. The disease is also called thrombosis of the visceral vessels, mesenteric infarction, intestinal ischemia.
For what reasons does intestinal infarction develop, what is it and how to treat it?
The mechanism of development of the disease
The mesentery, or mesentery, is a fold, consisting of two sheets of the peritoneum, with which the hollow organs of the abdominal cavity are attached to the back wall of the abdomen. In the thickness of the mesentery lie the mesenteric arteries, which provide blood supply to the intestines (see photo). The branches of the mesenteric vessels are interconnected by means of anastomoses, which provide the possibility of collateral circulation.
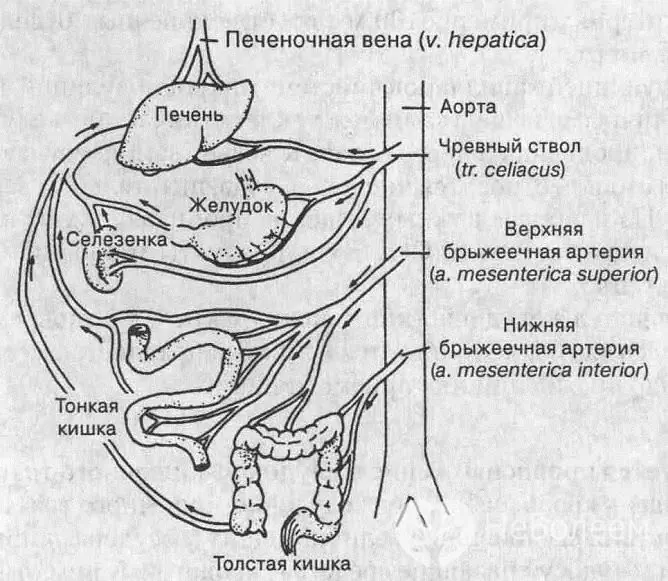
A heart attack occurs when blood flow is disturbed in one of the vessels feeding the intestines
In case of impaired blood circulation in the mesenteric vessels, occlusion of the arteries occurs, a sharp decrease or complete cessation of blood flow in them and ischemia of certain parts of the intestinal tract. As a result, the tissues of a certain part of the intestine receive insufficient oxygen and nutrients and die, that is, necrosis occurs. The necrotic tissue softens, the intestine is perforated, through the opening that has arisen, the contents of the intestine enter the abdominal cavity. As a result, peritonitis develops, acute inflammation of the peritoneum - a serious condition that threatens death.
Causes and risk factors
Usually, ischemia of the intestinal vessels occurs against the background of the progression of cardiovascular pathology in people over 70 years old. In older women, mesenteric infarction occurs twice as often. Taking into account the elderly age of patients and the presence of concomitant diseases in them, the decision on the surgical tactics of treatment can be quite difficult. The preparation process for the operation is also delayed due to the objective difficulties in making a diagnosis. Despite the optimization of diagnostic and therapeutic methods, mortality in the case of acute mesenteric infarction among patients reaches 50-90%.
Etiological factors leading to blockage of the bloodstream of the mesentery are divided into two groups:
- thrombotic or embolytic - blockage of the openings of the mesenteric vessels by a thrombus or embolus that migrated from the proximal vascular bed. Atherosclerosis, erythremia, myocardial infarction or endocarditis, hypercoagulability (increased blood clotting), atrial fibrillation, nonspecific aortoarteritis, prolonged blood congestion, severe intestinal infection, purulent abscess, trauma can lead to mesenteric thrombosis;
- non - occlusive - impairment of blood flow, decreased blood flow through the visceral vessels. The reasons for this condition can be: arterial hypotension, mesenteric vasospasm, decreased cardiac output fraction, massive blood loss, congestive heart failure, dehydration.
Often, mesenteric infarction develops as a result of the simultaneous action of several causal factors.
The risk of developing the disease is increased by:
- advanced age (over 60 years for women, 70 for men);
- sedentary lifestyle;
- prolonged dehydration;
- arrhythmias and other pathologies of the heart and blood vessels;
- heart surgery;
- myocardial infarction;
- cirrhosis of the liver (leads to increased pressure in the portal vein);
- chemotherapy.
Classification
To determine the most effective treatment plan, it is important to know the complete diagnosis, including the form and stage of the heart attack. The disease is classified according to the course, location and degree of circulatory disorders, the prevailing symptomatology.
Acute and chronic forms of the disease are distinguished along the course.
Depending on the vessels in which the circulatory disorder has occurred, there are three types of heart attacks:
- arterial - blood flow is disturbed in the mesenteric arteries; in most cases, this leads to a heart attack in 6-8 hours;
- venous - damage occurs in the mesenteric veins, such a violation does not lead to a heart attack immediately, but after 1-4 weeks;
- mixed - characterized by impaired blood flow, first in the arteries, and then in the veins.
By the degree of blood flow disturbance:
- compensated;
- subcompensated;
- decompensated heart attack.
Compensation is a process in which blood supply is maintained even if a vessel is damaged by additional vessels. With a compensated violation, the unaffected vessels completely take over the blood supply, with a subcompensated violation, the blood supply is not fully restored, with a decompensated one, the blood flow completely stops.

Mesenteric infarction is manifested by acute abdominal pain
Disease stages
In its development, mesenteric infarction goes through three stages replacing each other.
- Ischemic - circulatory disorders are reversible. Symptoms are nonspecific, which complicates the diagnosis.
- Necrotic - cells of the intestinal wall die from oxygen starvation resulting from ischemia.
- Stage of peritonitis - the intestinal wall collapses, the intestinal contents enter the abdominal cavity, an acute infectious inflammation of the peritoneum develops.
Bowel infarction symptoms
The clinical manifestations of mesenteric infarction are nonspecific and may differ depending on the stage, type and concomitant diseases.
Sometimes the onset of the disease is preceded by a period of precursors - the first signs of a developing heart attack, which patients often do not pay attention to or blame them on indigestion. In other cases, the symptoms of mesenteric infarction come on suddenly.
The patient is worried about intense pain in the abdomen - at first periodic, cramping, then constant. The localization of pain depends on which part of the intestine is affected. With a small intestine infarction, pain occurs in the central region or the right half of the abdomen, the large intestine in the left half, and the rectum in the lower left. On palpation, the abdomen is soft and slightly painful. In addition to abdominal pain, nausea, vomiting, and diarrhea occur. Auscultation of the abdomen reveals increased peristalsis, which subsides over several hours.
As the disease progresses, the patient's condition worsens, but at a certain point a period of imaginary well-being begins - the pain gradually weakens or disappears, but this is a bad prognostic sign, since it can speak of complete necrosis of the intestinal wall. With the progression of the disease, the phenomena of intoxication and dehydration increase. The skin becomes pale and dry, the tongue is dry, coated with a bloom. On palpation, the abdomen is swollen, but soft; in the abdominal cavity, a tightly elastic, low-displacement formation is determined - a swollen section of the intestine and mesentery. The patient becomes indifferent, lethargic, does not make contact.
Diagnostics
Diagnosis of intestinal infarction is based on instrumental methods. Ultrasound reveals a thickened intestinal wall and the presence of free fluid in the abdominal cavity. An ultrasound examination of blood vessels with an assessment of blood flow reveals a thrombus in one of the mesenteric vessels.
X-rays of the abdominal organs can show swollen bowel loops, but do not provide accurate information about the location of the blocked vessel. Angiography also belongs to the methods of radiography, however, it is considered more informative for the diagnosis. This method makes it possible to determine the exact location of the affected vessel, to identify the type and degree of blood flow disturbance.
Treatment
Treatment of mesenteric infarction should be started as soon as possible, the chances of the patient's survival and how serious the consequences will be depend on its timeliness. The goal of treatment is to eliminate the blockage of the vessel and remove the affected area of the intestine.
In the first hours after the onset of a heart attack, it is necessary to begin thrombolytic therapy, which helps to dissolve the blood clots that have blocked the vessel. Used drugs that activate fibrinolysis, i.e. resorption of blood clots - streptokinase, streptodecase, urokinase and other anticoagulants. At the same time, infusion therapy is started - intravenous infusion of drugs that stabilize blood circulation, replace the volume of circulating blood, and contribute to detoxification. In infarction caused by non-occlusive reasons, the administration of antispasmodics is indicated to improve visceral blood flow.
Attention! Photo of shocking content.
Click on the link to view.
The above methods refer to conservative therapy, and in this case they play an important but auxiliary role. In case of an intestinal infarction, surgery is required, and the less time it takes from the start of drug therapy to the operation, the higher the chances of a favorable outcome.
Surgical treatment consists in removing the affected area of the intestine, as well as restoring the blood supply to the affected area of the intestine. With peritonitis, the abdominal cavity is also washed with saline and antiseptics.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.