- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Pheochromocytoma

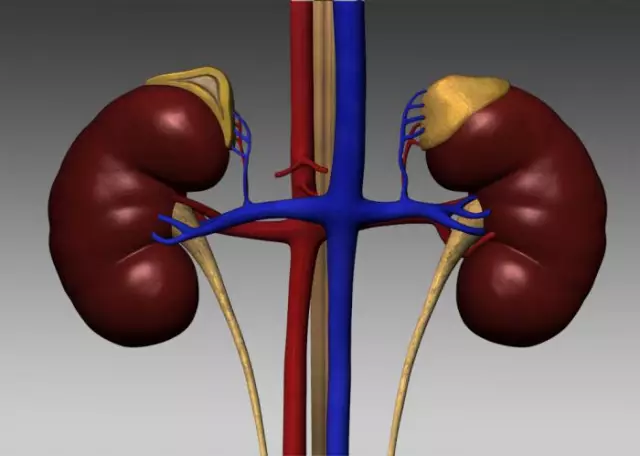
Pheochromocytoma is a hormone-active tumor of the adrenal gland. It is located in the medulla or chromaffin tissue of the gland and is considered one of the least studied endocrinological pathologies.
Many aspects of the etiology and development of adrenal pheochromocytoma are still unknown to modern medicine. The familial form of pheochromocytoma is characteristic of people with hereditary diseases: Recklinghausen's disease (aka neurofibromatosis), Sipple's or Hippel-Lindau's syndrome.
Pheochromocytoma occurs on average in 1 in 10 thousand people. Among people suffering from hypertension, the incidence of the disease is 1%, i.e. already 1 person per 100 patients with high blood pressure.
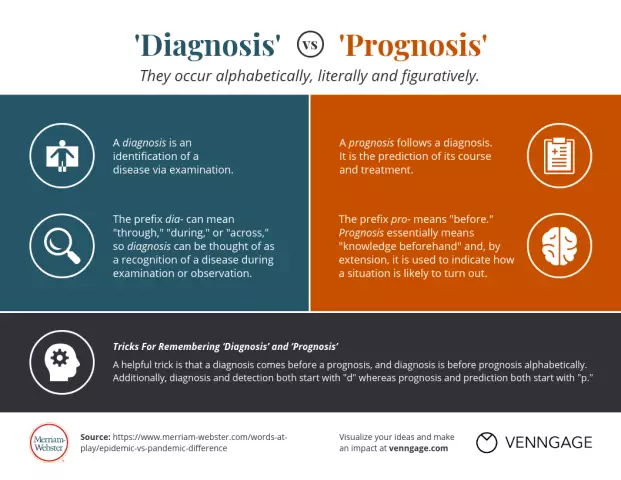
The difficulty in diagnosing adrenal pheochromocytoma lies in the often asymptomatic course of the disease or in a wide range of clinical symptoms of pheochromocytoma. So, according to American doctors, the correct diagnosis in patients with pheochromocytoma is established only in 37-40% of cases.
Typically, the adrenal pheochromocytoma is located in one of the glands. A tumor affecting both paired organs or localization of a pheochromocytoma outside the adrenal glands is diagnosed only in 10-15% of diseases.
And in another 10% of cases of pathology, malignant symptoms of pheochromocytoma are found - tumor metastasis to the lymph nodes, bones, muscles, liver, less often to the lungs and brain.
Adrenal pheochromocytoma symptoms
One of the main symptoms of pheochromocytoma is hypertension. High blood pressure in a patient can be episodic or constant. In the first case, bouts of hypertension provoke emotional distress, increased physical activity or overeating.
Symptoms of pheochromocytoma during an attack of hypertension include:
- throbbing headache,
- nausea
- vomiting
- pallor of the skin,
- sweating
- discomfort in the chest and abdomen,
- leg muscle cramps.
After an attack, the patient has a complete disappearance of all symptoms of pheochromocytoma, a sharp drop in blood pressure up to a cardinally opposite state - hypotension.
Differential diagnosis of pheochromocytoma should be carried out in people with complaints of:
- anxiety attacks,
- hyperventilation syndrome,
- hot flashes during menopause,
- increased need for caffeine,
- convulsions
- short-term loss of consciousness.
Among the symptoms of a complicated pheochromocytoma, there are signs of neuropsychic, cardiovascular, endocrine metabolic, hematological and gastrointestinal disorders:
- psychosis,
- neurasthenia,
- heart failure,
- vascular lesions of the kidneys and fundus,
- hyperglycemia (high blood glucose),
- hypogonadism (deficiency of hormones-androgens in the body),
- increased erythrocytes or blood ESR,
- drooling, etc.
Diagnostics of the adrenal pheochromocytoma
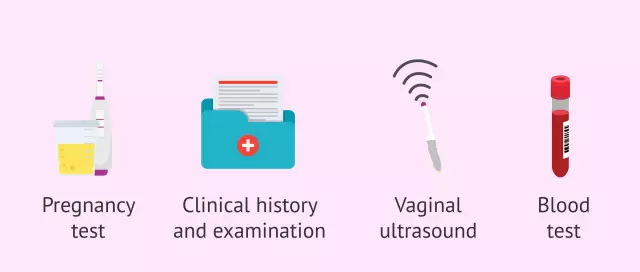
The clinical symptom of pheochromocytoma is the presence of catecholamines in the tissues of the urinary system, adrenal glands and bronchi. These specific substances produce catecholamine-producing tumor tissues. Granules of catecholamines in the diagnosis of pheochromocytoma can be detected using the method of silvering according to Gamperl-Masson and according to Grimelius.
The laboratory diagnosis of pheochromocytoma is also based on the assessment of the secretion of catecholamines in the daily portion of urine. In addition, adrenaline and vanillyl mandelic acid are often found in the patient's urine.
The second stage in the diagnosis of adrenal pheochromocytoma is to study the characteristics of the patient's arterial pressure fluctuations. Patients with this type of hormone-dependent tumor usually show an increase in total vascular resistance and a decrease in blood volume.
An obligatory stage in the diagnosis of pheochromocytoma is the control of cardiac activity. The characteristic symptom of pheochromocytoma is the development of cardiomyopathy and persistent heart rhythm disturbances.
After clinical and laboratory studies, topical diagnosis of pheochromocytoma is carried out - scintigraphy with a radioactive substance metaiodbenzylguanidine. MRI and CT are also effective methods for diagnosing pheochromocytoma with 90-100% sensitivity to a tumor.
The use of ultrasound in the diagnosis of pheochromocytoma is justified only if the tumor is more than 2 cm. Angiography in the diagnosis of pheochromocytoma is rarely used due to the laboriousness of the method and the high risk of complications.
Treatment of adrenal pheochromocytoma

The most radical treatment for pheochromocytoma is surgical removal of the tumor. However, it can be performed only after the blood pressure has stabilized.
For this purpose, at the preoperative stage of pheochromocytoma treatment, the patient is prescribed a-adrenergic blockers: Phenoxybenzamine, Phentolamine, Tropafen, etc. The criterion for the effectiveness of treatment of pheochromocytoma is the appearance of orthostatic fluctuations in blood pressure caused by a change in body position.
The choice of the method of surgical treatment of pheochromocytoma depends on the characteristics of the tumor. Good manipulation during the operation is provided by transperitoneal, transthoracic, extraperitoneal, or combined approaches for surgery.
In single tumors, the effectiveness of surgical treatment of pheochromocytoma is high. Relapse of the disease is observed only in 12-15% of cases.
In some cases, after removal of the tumor, the patient does not have a decrease in pressure. Such a postoperative complication is associated with damage to the renal artery or incomplete removal of the tumor.
In multiple tumors, there is no single standard in the surgical treatment of pheochromocytoma. Complete removal of all tumors is considered advisable, however, due to the high risk of surgery, this tactic of treating pheochromocytoma has to be abandoned and the tumors must be resected in several stages or only part of the tumor removed.
Conservative treatment of adrenal pheochromocytoma is less effective. It is aimed at reducing the level of catecholamines in the body with drugs based on A-methyltyrosine. Conservative treatment of pheochromocytoma can reduce the amount of catecholamines by 80% and prevent the development of a hypertensive crisis. However, the systematic intake of A-methyltyrosinoma can lead to mental disorders and functional disorders of the gastrointestinal tract.
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!