- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Glioma
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Glioma is the most common primary brain tumor originating from neuroglia cells (auxiliary cells in nerve tissue).

Glioma - brain tumor
Among all brain tumors, gliomas account for 60%. Favorite localization - the area of the chiasm (the intersection of the optic nerves) and the walls of the ventricles of the brain. Much less often gliomas are localized in the nerve trunks. Germination of gliomas into the meninges and the bones of the skull is extremely rare.
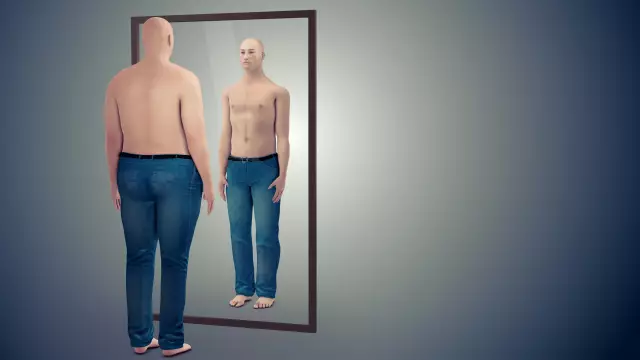
Gliomas are spindle-shaped or rounded, from 2-4 mm to 10 cm in diameter. They are characterized by slow growth and lack of metastasis, but at the same time they are capable of pronounced infiltrative growth, that is, germination into the surrounding tissues. It is not uncommon to find the boundary between healthy tissues and glioma even with a microscope. Another feature is the development of degenerative processes in the surrounding tissues. As a result, there is a discrepancy between the severity of neurological symptoms and the size of the glioma.
Causes and risk factors
Gliomas result from the uncontrolled growth and division of immature cells that make up the neuroglia.
Factors that increase the risk of developing glioma:
- Age. The disease occurs in people of any age, but people over 60 years of age are most susceptible to it.
- Radiation. There is evidence that previous radiation therapy increases the risk of developing glioma.
- Genetic predisposition. The likelihood of developing glioma increases significantly in people with mutations in the PDXDC1, NOMO1, WDR1, DRD5, and TP53 genes.
Forms of the disease
Neuroglial tissue is formed by three types of cells: ependymocytes, oligodendrogliocytes, and astrocytes. Depending on the cells that form the tumor, there are:
- astrocytomas;
- oligodendrogliomas;
- ependymomas;
- gliomas of mixed origin.

Glioblastoma multiforme, appearance
By the degree of malignancy, the following are distinguished:
- A benign tumor with slow growth, with no signs of malignancy (pleomorphic xanthoastrocytoma, subependymal giant cell astrocytoma, juvenile pilocytic astrocytoma).
- A so-called borderline, slowly growing tumor with one of the signs of malignancy, for example, the appearance of cellular atypia (diffuse astrocytoma).
- A tumor with two signs of malignancy other than necrosis (anaplastic astrocytoma).
- A tumor with at least three signs of malignancy, one of which is the presence of foci of necrosis (glioblastoma multiforme).
At the site of tumor localization there are:
- supratentorial (located above the cerebellum);
- subtentorial (located below the cerebellum).
Symptoms
Brain gliomas can have a wide variety of clinical manifestations, determined by size and location. The growth of glioma usually leads to the appearance of general cerebral symptoms:
- persistent headaches that cannot be stopped by taking non-steroidal anti-inflammatory drugs;
- frequent bouts of nausea, up to vomiting;
- a feeling of heaviness in the eyes;
- convulsive seizures.

One of the main symptoms of glioma is persistent headaches that cannot be stopped by NSAIDs.
General cerebral symptoms are most pronounced when glioma grows into the cerebral ventricles or cerebrospinal fluid pathways. In this case, the outflow of cerebrospinal fluid is disrupted, intracranial pressure increases, hydrocephalus develops.
Gliomas damage one or another area of the brain, which is manifested by the following focal symptoms (i.e., varying depending on the location of the tumor):
- visual impairment;
- speech disorders;
- vestibular ataxia (wobbly gait, constant dizziness);
- paresis and paralysis of the limbs;
- sensitivity disorders;
- memory impairment, concentration;
- thinking disorder;
- behavior disorders.
Diagnostics
Initial diagnosis of glioma requires a thorough neurologic examination. As the symptoms are varied, it may be necessary to consult a related specialist (eg, an ophthalmologist).
To assess the transmission of nerve impulses and the state of the neuromuscular system as a whole, electroneurography and electromyography are shown.

MRI or CT is indicated to diagnose glioma
An analysis of the cerebrospinal fluid obtained during the lumbar puncture is performed for the presence of atypical cells. Lumbar puncture is also necessary when performing ventriculography and pneumomyelography.
Visualization methods are applied:
- computed or magnetic resonance imaging;
- ultrasound scanning of the brain (M-echo);
- cerebral contrast angiography;
- daily EEG monitoring;
- scintigraphy;
- positron emission tomography.
Treatment
Complete surgical removal of cerebral glioma is possible only if the tumor is absolutely benign (grade I). In all other cases, gliomas quickly invade the surrounding tissues, which complicates the task. The use of MRI scanning, intraoperative brain mapping, and microsurgical techniques during surgery allows glioma resection within healthy tissues to be carried out as fully as possible, which significantly reduces the risk of disease recurrence.

If the glioma is benign, complete surgical removal is indicated
Contraindications to surgical treatment:
- severe general condition of the patient;
- inoperable localization of glioma;
- germination of glioma in both hemispheres of the brain;
- the presence of malignant tumors of other localization.
Gliomas are sensitive to radiation therapy and chemotherapy. Radio and chemotherapy are used both as independent methods of treatment (in the case of an inoperable tumor), and as an adjunct to surgery - in the preoperative period in order to reduce the tumor and after surgery in order to reduce the risk of disease recurrence.
Possible complications and consequences
As gliomas grow, they compress the structures of the brain and increase intracranial pressure. Clinically, this is manifested by the emergence and growth of neurological symptoms, which are persistent.
A complication of surgical treatment is bleeding in the tumor bed.
A distant consequence of traditional radiotherapy may be memory impairment of varying severity.
Forecast
The prognosis is generally poor. Due to the impossibility of complete removal of the tumor, the disease quickly recurs.
With a high degree of malignancy, 50% of patients die within the first year from the moment of diagnosis, only 25% live for more than two years.
After surgical removal of grade I gliomas, with minimal postoperative neurological complications, about 80% of patients live for more than five years.
Prevention
Specific prevention of the development of gliomas has not been developed.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!