- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Dorsal herniated disc
The content of the article:
- Features of the disease
- The reasons
- Symptoms
- Diagnostics
-
Treatment
- Conservative therapy
- Surgery
- Video
Dorsal hernia is a protrusion of deformed elements of the intervertebral disc (annulus fibrosus, nucleus) directly towards the spinal canal. This variant of the pathology is the most dangerous of all, since the nerve roots that lie in the immediate vicinity of the spinal cord are traumatized.

Dorsal hernia is the most dangerous form of intervertebral hernia, because it most injures the nerve roots
Features of the disease
- Has a strictly medial location relative to the axis of the vertebrae (exactly in the center).
- It can occur at any level of the spinal column, but more often at the L5 S1 level (lumbar spine).
- It can cause severe narrowing of the spinal canal, which leads to the formation of a severe condition - cauda equina syndrome.
- The first symptoms can occur in organs and tissues innervated by the compressed nerve. This phenomenon is especially clear when the cervical and thoracic regions are affected (tingling and numbness of the extremities, ringing in the ears and loss of visual acuity).
- There are no typical and classical manifestations of hernias, and in the presence of concomitant diffuse diseases of the spine, some difficulties arise in differential diagnosis.
There is no unified classification of hernias (it is divided according to the level of occurrence, the degree of damage to the intervertebral disc). Depending on the phase, a specific type of hernia and further treatment tactics are established.
The reasons
The causes of dorsal disc herniation of the lumbar spine and hernias of other departments:
| Cause | Features of formation |
| Dysplasia of the lumbosacral spine | Refers to congenital diseases that are associated with a violation of the development of the musculo-ligamentous apparatus and cartilage tissue, resulting in a change in the shape of the vertebrae (dorsal protrusion). |
| Osteochondrosis | In this case, the pathology may be the result of a prolonged degenerative-dystrophic process, or may occur in parallel with it. |
| Traumatic injury | In this case, the hernial protrusion occurs acutely due to a sharp violation of the intervertebral region (fractures or ruptures). As a rule, it requires urgent surgical treatment. |
| Infectious processes in the bones (chronic osteomyelitis, tuberculosis) | Prolonged infectious processes make bone structures fragile and often hollow from the inside. With minor loads, a fracture or shift of the vertebrae occurs with the formation of a hernial protrusion. |
| Prolonged intense exercise | The main load falls on the lumbar spine, hence the high incidence of pathology in this particular area. This category includes athletes, movers. |
Factors contributing to the occurrence of a hernia include:
- Scoliosis 3-4 degrees. With a significant shift of the vertebrae relative to the axis (more than 30 degrees), favorable conditions may arise for hernial protrusion.
- Metabolic disorders (obesity). It leads to tissue malnutrition and increased stress on the spinal column.
- Age-related changes in bone and cartilage tissue. Natural processes of thinning of bone structures due to the gradual leaching of calcium and phosphorus. For this reason, as a prevention of osteoporosis in the elderly, a course of vitamin and mineral therapy is indicated every six months.
- Physical inactivity. Particularly susceptible to pathology are people whose profession is associated with prolonged sitting (drivers, accountants, etc.).
- Heredity. There are not enough clinical studies to accurately state the relationship.
Symptoms
Dorsal medial hernias are mainly radicular symptoms and to a lesser extent local. Typical syndromes:
- Pain syndrome. It can be localized directly in the affected segment or irradiate to nearby areas. The pain increases with the growth and destruction of the hernial protrusion. When the deformed areas of the disc exit into the cavity of the spinal canal, intense pain can provoke a state of shock.
- Impaired motor function due to impaired innervation and reflex muscle spasm. The range of active and passive movements is sharply limited.
- Violation of all types of sensitivity (proprioceptive, pain, temperature, interoceptive). Since it is the root segment of the innervation that falls out, the sensitivity is lost in the whole area (upper limbs, lower limbs, abdomen, perineum, internal organs).
- Radicular syndrome is associated with a dysfunction of the abdominal or thoracic organs, as well as the pelvic cavity (depending on the specific level of damage).
- Myelopathic syndrome. It arises as a kind of complication in patients with a pronounced dystrophic process. It is formed when the lumen of the spinal canal narrows and is a combination of lower paraparesis, flaccid paresis in the hands and conductive sensory disorders.
In addition, coordination disorders, paresthesias, loss of deep sensitivity and dysfunction of the pelvic organs can be observed.

One of the symptoms is intense pain
Diagnostics
With dorsal diffuse disc herniation, the same diagnostic measures are shown as for other types of hernias. Diagnostics includes the following methods:
- Consultation with a neurosurgeon and a neurologist (collection of complaints, anamnesis, physical examination).
- Spondylography (X-ray of the spine). Indirect indicators of a hernia are considered to be a decrease in the intervertebral space, proliferation of the lateral surfaces of the vertebrae, signs of ossification of the articular surfaces, narrowing of the spinal canal, and instability of the vertebrae.
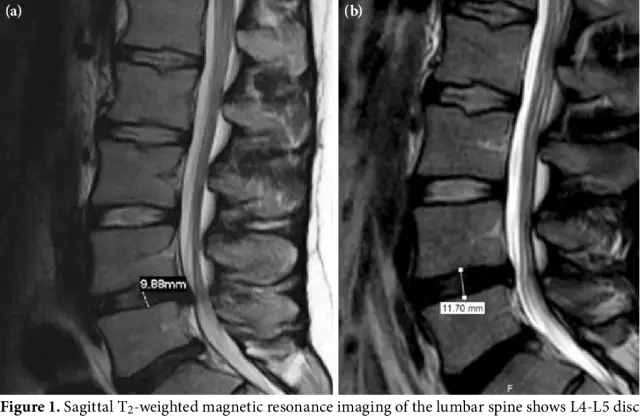
- MRI. Allows you to accurately establish the phase of the process (protrusion, prolapse, sequestration), and also determine the specific localization of the hernial protrusion (lateral, medial, lateral, paramedian). It is used for differential diagnosis in the case of osteophytes and disc protrusions (the osteophyte has a more intense signal than the contents of the hernial protrusion).
- CT. Optimally shows ischemic lesions of the spinal cord and makes it possible to identify the narrowing of the spinal cord.
Treatment
Hernia treatment begins with conservative measures. Surgery is required in less than 20% of patients.
Conservative therapy
Drug treatment includes:
- pain relievers - in order to muffle pain syndrome (do not completely relieve pain);
- non-steroidal anti-inflammatory drugs and chondroprotectors - are used to prevent inflammatory and degenerative phenomena;
- muscle relaxants - to relieve local muscle spasm;
- blockades (novocaine and lidocaine) - allow you to almost completely stop pain, but have a high risk of complications.
Surgery
Surgical treatment is indicated only for large hernias and the absence of positive dynamics when using different combinations of conservative methods. More often done under endotracheal anesthesia.
| Operation type | Description |
| Microdiscectomy | Ideal for dorsal hernias, it provides wide access to any part of the affected joint. It is carried out using high-tech equipment and has high efficiency. The average duration of the postoperative period is 5 days. In the postoperative period, wearing special orthopedic corsets is indicated. |
| Microendoscopic discectomy | The technique resembles the previous one and also allows you to remove almost any hernia. The difference lies in the lack of wide access (the operation is performed through a small puncture into which the endoscope is inserted). A less traumatic treatment option with a postoperative period of 3-4 days. |
| Percutaneous endoscopic lumbar discectomy | Option to remove a hernia with a lumbar position. It has a wider range of approaches (intralaminar, posterolateral, and transforaminal), which provides some mobility of the operating field. Optimal method for unaltered hernias. Not suitable for sequestration. |
After any option of surgical treatment, a long (up to 3 months) course of rehabilitation is required.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.