- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Extensive heart attack: consequences and chances of survival
The content of the article:
- Potential consequences of extensive myocardial infarction
-
Complications of a heart attack
- Cardiogenic shock
- Reperfusion syndrome
- Dressler's syndrome
- Extensive heart attack: risk groups
- First aid
- Video
The consequences of a massive heart attack are dangerous to the patient's health not only in the acute period, but also in the next few months or even years. However, high mortality is observed mainly due to complications - unexpected and polyetiological deterioration in health.
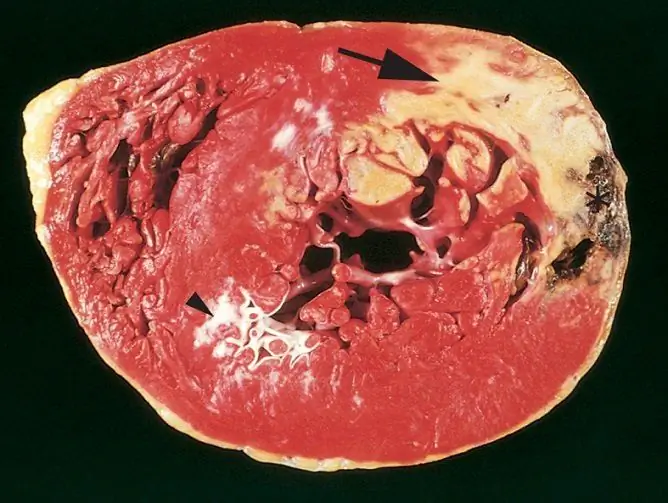
What is it - a massive heart attack? An extensive infarction is called a heart attack that is caused by a circulatory disorder in a large coronary vessel that carries a large volume of blood. Therefore, in the area fed by it, there is an acute lack of nutrients, and the cells quickly die. When most of the heart muscle falls out of the heart cycle, the consequences of such a heart attack can be very serious. Starting with the work of the heart itself and ending with organ failure, dysfunction in one way or another will affect each of the body systems.

To reduce the risk of complications, a patient with suspected heart attack should be taken to the hospital as soon as possible
Potential consequences of extensive myocardial infarction
In the clinic, the consequences of a heart attack are divided into cardiac, associated with disorders of the heart itself, and systemic, which arise as a result of heart failure and affect the circulatory system as a whole. And if the presence of complications after a heart attack depends, first of all, on the volume of medical care provided (the more time has passed from the moment of the attack to the arrival of an ambulance, the statistically lower the survival rate), then complete rehabilitation without any consequences after a massive heart attack is practically impossible.
The mechanism of development of dysfunction is as follows: due to necrosis of the myocardium, it, to one degree or another, loses the ability to contract, to conduct an impulse. When the acute phase of the attack ends and the patient is no longer threatened with instant death, the affected area is replaced by connective tissue. This structure is the main auxiliary component of body tissues, it fills in any damaged areas, while maintaining their structural integrity. Unfortunately, this cannot be said about the function of the organ - connective tissue is just a filler, deprived of the ability to contract. The heart loses strength, throws out less blood, which cannot but affect the rest of the body.
After a massive heart attack, the following heart effects are observed:
- Heart failure is a condition when the heart cannot adequately and fully perform its pumping function. It does not throw enough blood into the vessels, because of this, hemodynamics, pressure are disturbed, and starvation of cells in other organs begins. Blood can also stagnate in the veins due to the low speed of movement, remain in the chambers of the heart itself. Acute heart failure develops during the heart attack itself, and chronic heart failure remains after the manifestation of the disease for the rest of his life. All subsequent violations are connected with it.
- Cardiosclerosis is the proliferation of connective tissue in the thickness of the muscle. Since it does not have the necessary properties, the heart wall loses its inherent strength. Under blood pressure, it can stretch, bulge. In the case of uneven expansion of one section of the wall, they speak of an aneurysm of the heart, and uniform and all-round expansion of the chambers of the heart together with the depletion of their walls is called dilatation. Both of these conditions increase the risk of heart failure with intense exercise or high blood pressure.
- Rhythm and conduction disturbances - since the pathways in the heart are disturbed, in the vast majority of cases, patients complain of arrhythmias, extrasystoles (extraordinary contractions), a feeling of cardiac arrest, tachycardia (high heart rate). Sometimes these pathologies are exacerbated by ventricular fibrillation, which is a life-threatening condition.
- Blood clots - a common consequence of a massive heart attack is a blood clot in one of the chambers of the heart or in the great vessel. This is due to the fact that blood flow slows down, and the damaged endothelium of the vascular wall creates conditions for intravascular coagulation. Thromboembolism is one of the most important causes of heart attack, including repeated, therefore, in the course of drug treatment, fibrinolytics are prescribed to each patient in the postinfarction period to prevent blood clots.
Systemic consequences:
- Pulmonary edema - occurs due to stagnation of blood in the pulmonary circulation. The pressure in the pulmonary artery rises significantly, and the lung tissue, one of the most densely penetrated by vessels, suffers from this in the first place. This is one of the first manifestations of heart failure, which is characterized by shortness of breath (depending on the degree of dysfunction, it can occur both during exertion and in a state of calm), productive cough, in the later stages - hemoptysis.
- Portal hypertension - has the same developmental mechanism as pulmonary, but in this case, the pressure increases in the portal vein of the liver. Large volumes of blood accumulate in the blood depot of the liver, it increases and begins to squeeze the surrounding organs. One of the symptoms of portal hypertension is ascites, a free fluid in the abdominal cavity that enters the intercellular space from overcrowded vessels.
Complications of a heart attack
The prognosis for extensive heart attack largely depends on whether complications have arisen or not.
For each of the complications, there is a period of vulnerability, during which the risk of its development is highest. During the course of the disease, the most acute, acute, subacute periods and the stage of scarring are distinguished. In the acute period, cardiogenic shock occurs, in the acute period - reperfusion syndrome, and in the subacute and during scarring, postinfarction syndrome is likely, also known as Dressler's syndrome.
Cardiogenic shock
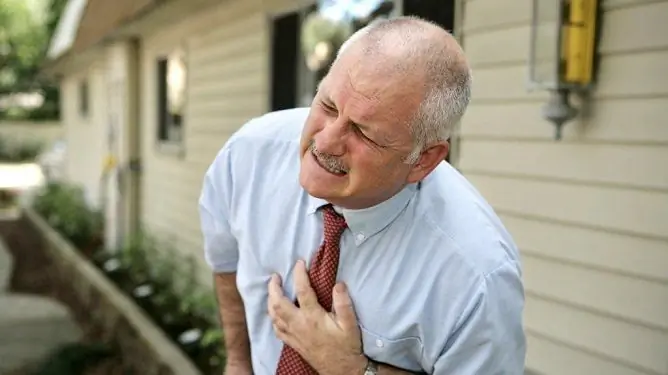
This condition is accompanied by acute chest pain and occurs in the first hours after a heart attack. Cardiogenic shock occurs when the pumping function of the heart drops sharply, and due to a stressful situation and the release of biologically active substances from the affected tissues, peripheral vessels contract. At this point, peripheral resistance increases, cells begin to starve, and shock-sensitive organs are damaged. The reverse mechanism is triggered - a strong vasodilation. It leads to a sudden drop in blood pressure, collapse. The patient is in a state of shock, may faint.

Cardiogenic shock, like the heart attack itself, is accompanied by intense, often unbearable pain in the heart
Reperfusion syndrome
Reperfusion syndrome is a more distant complication, but no less dangerous. It occurs when, after a heart attack, a large amount of drugs are administered that dissolve dense blood clots, i.e., fibrinolytics. The tissue under conditions of prolonged ischemia has accumulated a large amount of toxic substances. When fresh blood suddenly flows to it, these metabolites enter the bloodstream, and the affected area expands even more. Therefore, fibrinolytic drugs should be strictly dosed.
Dressler's syndrome
Dressler's syndrome, or postinfarction syndrome, occurs later than other complications. How is it dangerous? This is an autoimmune reaction of the body to damaged tissue, which develops several weeks after a heart attack. The immune system recognizes the dead tissue of the heart muscle as foreign, producing antibodies on them. A systemic reaction occurs, which is manifested by a rise in temperature, weakness, a significant deterioration in well-being, but most importantly - an increase in the focus of necrosis. Inflammation can also spread to other structures of the heart, causing postinfarction pericarditis or endocarditis.
The main task of therapy is to prevent the development of complications. With the implementation of pathogenetic treatment, the chances of surviving the consequences of an extensive heart attack increase. This is evidenced by medical sources and reviews of patients who have suffered an illness.
Extensive heart attack: risk groups
The disease develops more often in people who are exposed to risk factors. These are lifestyle and behavioral features that significantly increase the likelihood of a heart attack. These include:
- overweight;
- inappropriate nutrition (excessively high content of fats and carbohydrates in the diet);
- atherosclerosis of the coronary vessels (atherosclerotic plaque narrows the lumen of the vessel, blocks the blood flow, and also contributes to the formation of blood clots);
- male sex (female sex hormones have a protective effect on blood vessels);
- age (after 40 years, the risk of the disease begins to grow and reaches a peak at 60 years - at this age, the frequency of heart attack becomes the same for men and women. In older people at 80, the incidence decreases again);
- thrombus formation (blood clots can develop not only as a result of atherosclerosis, but also after abdominal operations, as well as while taking combined oral contraceptives);
- arterial hypertension (significantly worsens the condition of the vascular wall due to constant pressure on it, can lead to rupture and hemorrhagic infarction);
- bad habits - alcohol abuse and smoking;
- hypodynamia.
In many ways, the chances of recovery depend on the exclusion of risk factors in the post-infarction period, because otherwise the damaging agent continues to act after the attack. Statistics show that 30% of people after a myocardial infarction develop a second heart attack within a year.
First aid
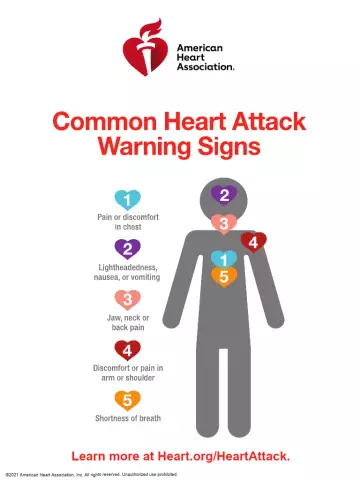
The size of the necrosis focus, and hence the chances of survival, depends on emergency care in the first hours after an attack. There are a number of sequential steps to take if a person makes the following complaints:
- acute burning pain behind the sternum, which radiates between the shoulder blades, in the neck, arm, sometimes in the stomach, fingertips;
- increased and / or uneven heartbeat, a feeling of cardiac arrest;
- dyspnea;
- weakness, dizziness;
- sweating.
The patient can hold on to his heart, say that he is hot in the room. In this case, a heart attack can be suspected. The algorithm of actions is as follows:
- Call an ambulance. The sooner she arrives, the earlier the ECG will be done and the drugs administered. Is it possible to provide medical assistance at home? Unfortunately not - the presence of medical personnel and special medicines is mandatory.
- Calm the patient down, sit him down.
- Open all windows in the room, remove excess clothing, loosen tight belts and buckles.
- Give a tablet of Nitroglycerin under the tongue - this drug helps with angina pectoris, with a heart attack, its effectiveness is lower, however, it dilates blood vessels and somewhat softens oxygen starvation of myocardial cells.
- Give aspirin - regular or Aspirin-Cardio will do. This is necessary to thin the blood and prevent blood clots.

The first thing to do if you suspect a heart attack is to call an ambulance.
You cannot leave the patient alone, the ambulance team who has arrived must be told when the attack began, how it manifested itself, how long and what drugs the patient received. If an ambulance cannot arrive quickly for some reason, it is necessary to deliver the patient to the hospital by yourself, by car.
In a hospital setting, examinations will be carried out - ECG and EchoCG, which will determine the stage of the heart attack, the degree of damage, the localization of the necrosis focus. A biochemical blood test for markers of specific inflammation will confirm the diagnosis of a heart attack. At the same time, fibrinolytics, antianginal agents, anticoagulants are administered. Additionally, sedatives are prescribed.
All these measures, carried out in a timely manner, significantly increase the patient's chances of surviving a massive heart attack.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.