- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Pituitary adenoma
The content of the article:
- Causes and risk factors
- Forms of the disease
- Pituitary adenoma symptoms
- Diagnostics
- Treatment of pituitary adenoma
- Possible complications and consequences
- Forecast
- Prevention
A pituitary adenoma is a benign neoplasm from the glandular tissue of the anterior pituitary gland.

Signs of a pituitary adenoma
The pituitary gland is the central organ of the endocrine system, along with the hypothalamus, with which it has a close connection. It is located at the base of the brain in the pituitary fossa of the sella turcica, has anterior and posterior lobes. The hormones secreted by the pituitary gland affect growth, metabolism, and reproductive function.
In the structure of all intracranial neoplasms, the proportion of pituitary adenoma is 10-15%. Most often, the disease is diagnosed at the age of 30-40, it also occurs in children, but such cases are rare. Pituitary adenoma in men occurs with approximately the same frequency as in women.
Causes and risk factors
The reasons for the development of pituitary adenoma are not completely clear. There are two theories explaining the mechanism of tumor development:
- Internal defect. According to this hypothesis, gene damage in one of the cells of the pituitary gland gives rise to its transformation into a tumor, followed by growth.
- Disorder of hormonal regulation of the functions of the pituitary gland. Hormonal regulation is carried out by the hypothalamic releasing hormones - liberins and statins. Presumably, with hyperproduction of liberins or hypoproduction of statins, hyperplasia of the glandular tissue of the pituitary gland occurs, which gives rise to the tumor process.

Traumatic brain injury can lead to the development of a pituitary adenoma
Risk factors for the development of the disease include:
- traumatic brain injury;
- neuroinfections (neurosyphilis, poliomyelitis, encephalitis, meningitis, brain abscess, brucellosis, cerebral malaria, etc.);
- long-term use of oral contraceptives;
- adverse effects on the developing fetus during intrauterine development.
Forms of the disease
Pituitary adenomas are classified into hormonally active (produce pituitary hormones) and hormonally inactive (do not produce hormones).
Depending on which hormone is produced in excess, hormonally active pituitary adenomas are divided into:
- prolactin (prolactinomas) - develop from prolactotrophs, are manifested by increased production of prolactin;
- gonadotropic (gonadotropinomas) - develop from gonadotrophs, are manifested by increased production of luteinizing and follicle-stimulating hormones;
- somatotropic (somatotropinomas) - develop from somatotrophs, are manifested by increased production of somatotropin;
- corticotropic (corticotropinomas) - develop from corticotrophs, are manifested by increased production of adrenocorticotropic hormone;
- thyrotropic (thyrotropinomas) - develop from thyrotrophs, are manifested by increased production of thyroid-stimulating hormone.
If a hormonally active pituitary adenoma secretes two or more hormones, it is referred to as mixed.

Hormone-dependent pituitary adenomas produce pituitary hormones
Hormonally inactive pituitary adenomas are subdivided into oncocytomas and chromophobic adenomas.
Depending on the size:
- picoadenoma (diameter less than 3 mm);
- microadenoma (diameter no more than 10 mm);
- macroadenoma (diameter more than 10 mm);
- giant adenoma (40 mm or more).
Depending on the direction of growth (in relation to the Turkish saddle), pituitary adenomas can be:
- endosellar (growth of neoplasms in the cavity of the sella turcica);
- infrasellar (the spread of the neoplasm is lower, it reaches the sphenoid sinus);
- suprasellar (spread of the tumor upward);
- retrosellar (posterior growth of the neoplasm);
- lateral (spread of the neoplasm to the sides);
- ansellar (anterior growth of the tumor).
When a neoplasm spreads in several directions, it is called in those directions in which the tumor grows.
Pituitary adenoma symptoms
The onset of symptoms of a pituitary adenoma is due to the pressure of the growing tumor on the intracranial structures, which are located in the area of the sella turcica. With a hormonally active form of the disease, endocrine disorders prevail in the clinical picture. In this case, clinical manifestations are usually associated not with the very increased production of the hormone, but with the activation of the target organ, which the hormone acts on. In addition, the growth of the pituitary adenoma is accompanied by symptoms that occur due to the destruction of the pituitary tissue by an enlarging tumor.
Ophthalmic-neurological manifestations that occur with pituitary adenoma depend on the prevalence and direction of its growth. These symptoms include diplopia (visual impairment in which visible objects are bifurcated), changes in visual fields, and oculomotor disorders.

Diplopia refers to the ophthalmic-neurological manifestations of the pituitary adenoma
A headache appears due to the pressure of the neoplasm on the Turkish saddle. Painful sensations are usually localized in the eye area, in the temporal and frontal regions, do not depend on the position of the patient's body, are not accompanied by a feeling of nausea, have a dull character, do not stop or are mildly relieved by taking analgesic drugs. A sharp increase in headache may be associated with intense tumor growth or with hemorrhage in the neoplasm tissue.
With the progression of the pathological process, atrophy of the optic nerve develops. The growth of the neoplasm in the lateral direction leads to paralysis of the eye muscles caused by damage to the oculomotor nerves (ophthalmoplegia), which is accompanied by a decrease in visual acuity. Usually, visual acuity decreases first in one eye, and then in the other, however, simultaneous visual impairment in both eyes may occur. When the tumor grows into the bottom of the sella turcica and spreads to the ethmoid labyrinth or sphenoid sinus, nasal congestion appears (similar to the clinical picture with nasal neoplasms or sinusitis). With the growth of the pituitary adenoma upwards, disturbances of consciousness occur.

When the pituitary adenoma extends into the ethmoid labyrinth or sphenoid sinus, the patient develops nasal congestion
Endocrine metabolic disorders depend on which hormone is produced in excess.
With somatotropinoma in children, symptoms of gigantism are noted, and acromegaly develops in adults. Skeletal changes in patients are accompanied by diabetes mellitus, obesity, diffuse or nodular goiter. Often, there is an increased secretion of sebum with the formation of papillomas, nevi and warts on the skin, hirsutism (excessive male hair growth in women), hyperhidrosis (increased sweating).
With prolactinoma in women, the menstrual cycle is disturbed, galactorrhea appears (spontaneous milk release from the mammary glands, not associated with lactation), amenorrhea (absence of menstruation over several menstrual cycles), infertility. These pathological conditions can occur both in a complex and in isolation. Patients with prolactinoma have acne, seborrhea, and anorgasmia. With this form of pituitary adenoma in men, galactorrhea, gynecomastia (enlargement of one or both mammary glands), decreased sex drive, impotence are usually observed.

Prolactinoma in women is characterized by menstrual irregularities and galactorrhea.
The development of corticotropinomas leads to the appearance of a syndrome of hypercortisolism, increased skin pigmentation, and sometimes to mental disorders. Ophthalmic neurological disorders with corticotropinoma are usually not observed. This form of the disease is capable of malignant transformation.
With thyrotropinoma, patients may exhibit symptoms of hyper- or hypothyroidism.
Gonadotropinoma usually presents with ophthalmic-neurological disorders, which may be accompanied by galactorrhea and hypogonadism.
Of the common symptoms in patients with hormone-dependent tumors, weakness, rapid fatigue, decreased ability to work, and changes in appetite are noted.
Diagnostics
If a pituitary adenoma is suspected, patients are advised to undergo an examination by an endocrinologist, neurologist and ophthalmologist.
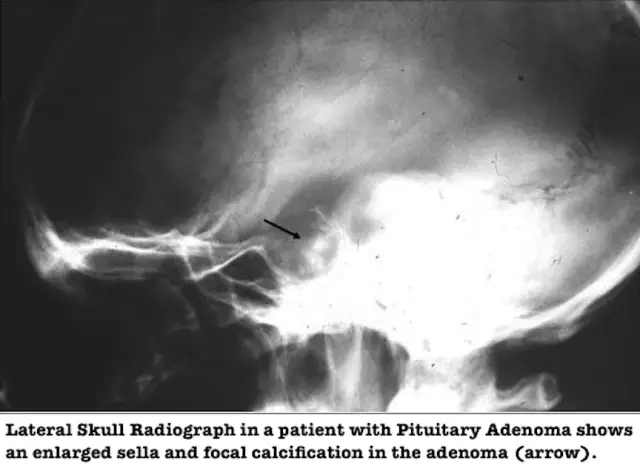
To visualize the tumor, an X-ray examination of the Turkish saddle is performed. At the same time, the destruction of the back of the Turkish saddle, the double-circuit or multi-contour of its bottom are determined. Turkish saddle can be increased in size and have a balloon-like shape. There are signs of osteoporosis.
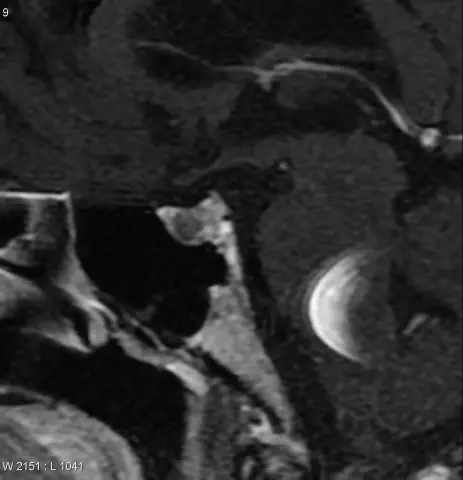
Sometimes additional pneumatic cisternography is required (allows to detect displacement of chiasmatic cisterns and signs of an empty Turkish saddle), computed tomography and magnetic resonance imaging. In 25-35%, pituitary adenomas are so small that their visualization is difficult even with the use of modern diagnostic tools.
If you suspect that the growth of the adenoma is directed towards the cavernous sinus, an angiography of the brain is prescribed.

Pituitary adenoma diagnosed by MRI of the Turkish saddle
Of no small importance for the diagnosis is the laboratory determination of the concentration of pituitary hormones in the patient's blood by the radioimmunological method. Depending on the existing clinical manifestations, it may be necessary to determine the concentration of hormones produced by the peripheral endocrine glands.
Ophthalmic disorders are diagnosed during an ophthalmological examination, checking the patient's visual acuity, perimetry (a method that allows you to explore the boundaries of the visual fields), as well as ophthalmoscopy (an instrumental technique for examining the fundus).
Exercise pharmacological tests can determine the presence of an abnormal reaction of adenomatous tissue to pharmacological effects.
Differential diagnosis is carried out with other brain neoplasms, side effects from taking certain medications (antipsychotics, some antidepressants, corticosteroids, antiulcer drugs), primary hypothyroidism.
Treatment of pituitary adenoma
The choice of treatment regimen for pituitary adenoma depends on the form of the disease.
With the development of a hormonally inactive pituitary adenoma of a small size, expectant tactics is usually justified.
Drug treatment is indicated for prolactinomas and somatotropinomas. Patients are prescribed drugs that block the excessive production of hormones, which helps to normalize hormonal levels, improve the psychological and physical condition of the patient.
Radiation therapy as the main method of treating pituitary adenoma is used relatively rarely, usually in cases where there is no positive effect of drug therapy and there are contraindications for surgical treatment.
The radiosurgical method is used to destroy a neoplasm by exposing the pathological focus to targeted high-dose ionizing radiation. This method does not require hospitalization and is atraumatic. Radiosurgical treatment is indicated if the optic nerves are not involved in the pathological process, the neoplasm does not go beyond the Turkish saddle, the Turkish saddle is of normal size or slightly enlarged, the tumor diameter does not exceed 3 cm, and there is also a refusal of the patient to carry out other types of treatment or contraindications to them conducting.
Radiosurgical action is used to remove the remnants of a neoplasm after surgery, as well as after remote irradiation (radiotherapy).

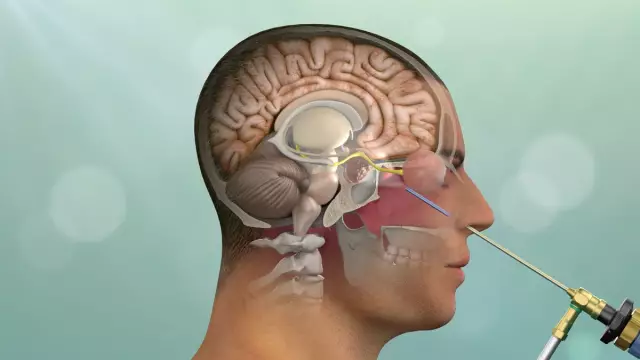
Removal of pituitary adenoma through the nasal passages
The indication for surgical removal of the pituitary adenoma is the progression of the tumor and / or the absence of a therapeutic effect after several courses of drug therapy for hormonally active tumors, as well as the absolute intolerance of dopamine receptor agonists.
Surgical removal of a pituitary adenoma can be performed by opening the cranial cavity (transcranial method) or through the nasal passages (transnasal method) using endoscopic techniques. Usually, the transnasal method is used for small pituitary adenomas, and the transcranial method is used to remove macroadenomas of the pituitary gland, as well as in the presence of secondary tumor nodes.
Transnasal removal of the pituitary adenoma is performed under local anesthesia. Access to the operating field is through the nostril, an endoscope is brought to the pituitary gland, the mucous membrane is separated, the bone of the anterior sinus is exposed, with a special drill, access to the Turkish saddle is provided. Then, parts of the neoplasm are sequentially removed. After that, the bleeding is stopped and the Turkish saddle is sealed. The average hospital stay after such an operation is 2-4 days.
When removing a pituitary adenoma by the transcranial method, access can be performed frontally (the frontal bones of the skull are opened) or under the temporal bone, the choice of access depends on the direction of growth of the neoplasm. Surgery is performed under general anesthesia. After shaving off the hair, projections of blood vessels and important structures are outlined on the skin, which are undesirable to touch during the operation. Then a soft tissue incision is made, bone is cut, and the dura mater is incised. The adenoma is removed with an electric forceps or an aspirator. Then the bone flap is returned to its place, and sutures are applied. After the end of the anesthesia, the patient spends a day in the intensive care unit, after which he is transferred to the general ward. The period of hospitalization after such an operation is 1-1.5 weeks.
Pituitary adenoma can negatively affect the course of pregnancy. If pregnancy occurs during treatment with dopamine receptor agonists, these drugs should be discontinued. Patients with a history of hyperprolactinemia have an increased risk of spontaneous abortion, therefore, such patients are advised to undergo natural progesterone therapy during the first trimester of pregnancy. Breastfeeding is not prohibited.
Possible complications and consequences
Complications of pituitary adenoma include malignancy, cystic degeneration, apoplexy. Lack of therapy for hormonally active adenoma leads to the development of severe neurological disorders and metabolic disorders.
Forecast
A pituitary adenoma is a benign neoplasm, however, some types of adenomas can take on a malignant course in unfavorable conditions. The possibility of complete removal of the pituitary adenoma depends on its size (with a tumor diameter of more than 2 cm, there is a possibility of postoperative relapse within five years after the operation) and its shape. Recurrences of pituitary adenoma occur in about 12% of cases. Self-healing is also possible, this is especially often observed with prolactinomas.
Prevention
In order to prevent the development of pituitary adenoma, it is recommended:
- avoid traumatic brain injury;
- avoid taking oral contraceptives for a long time;
- create all conditions for the normal course of pregnancy.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!