- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Lymphadenitis

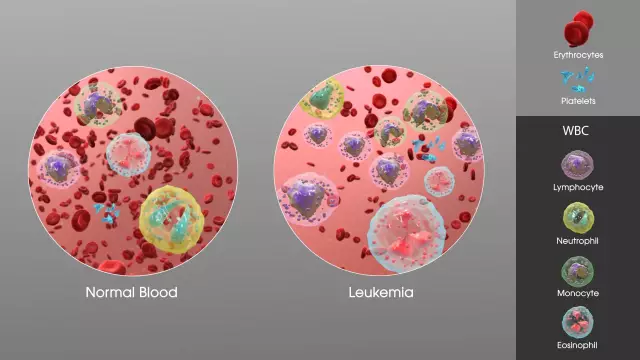
Lymphadenitis is an inflammation of the lymph nodes, often accompanied by a purulent process. The most common cause of lymphadenitis are streptococci and staphylococci, which enter the lymph nodes with lymphangitis. For the most part, lymphadenitis is localized in the armpit and groin. More often you can find lymphadenitis in children.
Lymphadenitis causes
The causative agent of the disease are pyogenic microorganisms, which from foci of purulent inflammation (panaritium, phlegmon, etc.) penetrate into the lymph nodes. This happens by direct contact with microorganisms, as well as through the blood or lymph.
Lymphadenitis can be purulent or non-purulent, and according to the duration of the course, acute or chronic lymphadenitis is distinguished. A purulent-inflammatory process can spread to one lymph node, or affect nearby ones. With purulent lymphadenitis, the formation of an extensive focus of suppuration in soft tissues is characteristic - adenophlegmon.
Lymphadenitis symptoms
A characteristic sign of lymphadenitis in children and adults is severe pain, which forces the patient to hold the limb in a certain position. The patient's body temperature rises and edema occurs. In the late stage of lymphadenitis, fluctuation and leukocytosis may develop.
Types of lymphadenitis
Lymphadenitis is acute, chronic, specific and non-specific.
The main cause of nonspecific lymphadenitis are staphylococci, streptococci, less often other pyogenic microbes and tissue decay products from primary foci of infection. Primary foci are purulent wounds, carbuncles, furuncles, erysipelas, thrombophlebitis, trophic ulcers, osteomyelitis, etc. Microbes and toxins enter the lymph nodes by contact, hematogenous and lymphogenous pathways. Also, microbes can penetrate directly into the lymph node when injured. In this case, lymphadenitis is the primary disease.
The ingress of microbes into the lymph nodes provokes an inflammatory process, as a result of which hemorrhagic, serous, fibrinous purulent lymphadenitis may occur. If you do not treat lymphadenitis, the disease can lead to irreversible processes - necrosis, abscess formation, ichorous decay of lymph nodes. At the initial stage of the disease, the endothelium sloughs off, the sinuses expand, and congestive hyperemia occurs.
In simple lymphadenitis, inflammation, as a rule, does not go beyond the lymphatic capsule. If the disease has a destructive form, the inflammatory process can spread to the surrounding tissues.
Nonspecific lymphadenitis can be acute or chronic.
Acute nonspecific lymphadenitis begins with headache, swollen lymph nodes, and soreness. Also, the symptoms of lymphadenitis include fever and general malaise. If the inflammatory process is not pronounced, then the general condition of the patients suffers little. There is soreness of the lymph nodes, their increase in size, induration. With the progression of the disease and the transition of the inflammatory process into a destructive form, all the symptoms of lymphadenitis increase. The pains become sharp, and the skin over the lymph nodes is hyperemic.
With the development of adenophlegmon, the general condition of patients deteriorates sharply. The body temperature rises sharply, sometimes to critical levels, tachycardia, chills, severe weakness, headaches occur.
Nonspecific acute lymphadenitis is fraught with the development of complications such as thrombophlebitis, the spread of a purulent process to the cellular spaces and metastatic foci of infection (lymphatic fistulas, septicopyemia).
Chronic nonspecific lymphadenitis in children and adults can occur from acute lymphadenitis or be the result of recurrent inflammatory diseases such as chronic tonsillitis, microtrauma, inflammation in the teeth, etc. As a rule, chronic lymphadenitis rarely turns into a purulent form.
Symptoms of chronic nonspecific lymphadenitis include: enlargement and thickening of the lymph nodes, which remain enlarged and slightly painful for a long time. Sometimes complications such as edema, lymphostasis, elephantiasis, and lymph circulation disorder occur.
The causes of specific lymphadenitis are mainly tuberculosis, syphilis, actinomycosis, plague and other diseases. So, for example, tuberculous lymphadenitis can most often be found in children during the period of primary tuberculosis.
In the acute stages of specific lymphadenitis, there is a strong increase in body temperature, an increase in lymph nodes, symptoms of intoxication of the body, inflammatory-necrotic processes in the lymph nodes.
Diagnosis of lymphadenitis
To diagnose the disease, the doctor looks at the patient's general clinical symptoms and anamnestic information.

To clarify the diagnosis, the patient is shown a puncture biopsy of the lymph node. In severe cases, it is possible to remove the lymph node for the purpose of histological examination.
Lymphadenitis treatment
The method of treatment of acute nonspecific lymphadenitis depends on the severity of the process. In the initial stages, predominantly conservative treatment is used. For the affected organ, complete rest, UHF treatment and adequate treatment of the focus of infection (drainage of the abscess, timely opening of abscesses and phlegmon, opening of purulent streaks) are shown. The patient is prescribed antibiotic treatment. Purulent lymphadenitis is mainly treated surgically: adenophlegmon, abscesses are opened, pus is removed, and wounds are drained.
Treatment of chronic nonspecific lymphadenitis is aimed at eliminating the underlying disease, which provoked lymphadenitis.
Specific lymphadenitis is treated depending on the nature of the damage to the lymph nodes and the severity of tuberculous changes in the organs. If the process is active, the patient is prescribed first-line drugs: streptomycin, tubazide in combination with ethionamide, PASK, pyrazinamide, protionamide, ethambutol. Treatment of specific lymphadenitis is long-term (up to one and a half years). With a pronounced purulent process, the patient is prescribed antibiotic therapy.
Prevention of lymphadenitis
First of all, for the prevention of lymphadenitis, it is necessary to try to avoid injuries, effectively fight wound infections and rationally and timely treat purulent-inflammatory diseases.
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!