- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Cryptorchidism
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Cryptorchidism is a pathological condition in which one or both testicles are located outside the scrotum (in the inguinal canal, abdominal cavity, under the skin).

The testicles are paired male gonads in which sperm and male sex hormones are produced. They are located in the scrotum, which is necessary for the maturation of spermatozoa, the condition of which is a lower temperature than in the abdominal cavity. Normally, they differ somewhat in size and are located at different levels (usually the right one is higher than the left one), easily move in the scrotum and can completely or partially go under the wall of the peritoneum. The testicles descend into the scrotum from the retroperitoneal space from the 6th month of intrauterine development until delivery. This sometimes happens during the first year of life.
Cryptorchidism is a common pathology, it is recorded in 3% of cases in full-term male children and in 30% of cases in premature babies, while in children of the second year of life, the testicles descend independently into the scrotum in 75 and 90% of cases, respectively. More often, right-sided cryptorchidism is observed, the bilateral accounts for 10-30% of all cases.
Causes and risk factors
The mechanism of development of cryptorchidism is not fully understood. The main causes of pathology are divided into two groups:
- mechanical obstacles to the advancement of the testicle: shortening of the testicular leash, fixation of testicular vessels in the deep inguinal ring by embryonic strands, shortening and underdevelopment of testicular vessels, underdevelopment of the inguinal canal, narrowness of the superficial and deep inguinal rings;
- dysfunction of the endocrine glands of the pregnant woman and the fetus: dysfunction of the pituitary and thyroid gland of the fetus, disruption of the endocrine function of the placenta, type 1 or 2 diabetes mellitus, etc.
Against the background of anatomical and mechanical factors, unilateral cryptorchidism is usually formed, hormonal factors, in turn, contribute to the development of a bilateral form of the disease.
Risk factors include:
- genetic predisposition;
- viral or bacterial infections suffered by a woman during pregnancy (especially toxoplasmosis, rubella, sexually transmitted infections, influenza);
- taking a pregnant woman of drugs from the group of non-narcotic analgesics;
- professional activities of a pregnant woman associated with toxic substances;
- bad habits in a pregnant woman;
- prematurity;
- fetal hypoxia, insufficient weight of the child.
Acquired cryptorchidism can develop with injuries to the scrotum and inguinal ring. Secondary cryptorchidism develops due to the slow growth of the spermatic cord, as a result of which the descended testicle is displaced from the scrotum.
False cryptorchidism occurs with a small diameter of the testicle in comparison with the diameter of the outer inguinal ring, while in the case of muscle contraction (with tension, cold), the testicle is pulled up to the inguinal fold.
Forms of the disease
Cryptorchidism is classified into congenital and acquired, true and false. In true cryptorchidism, the testicle cannot be moved into the scrotum when manually brought down. When false, regardless of the initial location of the testicle, it can be effortlessly brought back into the scrotum. False cryptorchidism accounts for about 50% of all cases of the disease.
Depending on the localization of the testicle, cryptorchidism is divided into three forms:
- intra - abdominal - the testicle is localized in the abdominal cavity proximal to the inner inguinal ring, occurs in 10% of cases;
- inguinal, or inguinal - the testicle is located between the outer and inner inguinal rings in the inguinal canal;
- ectopia of the testicle - the testicle is located outside its usual path of descent into the scrotum distal to the inner inguinal ring, most often in the groin, perineum, on the thigh, at the root of the penis, is recorded in 5% of cases.
In addition, cryptorchidism can be primary and secondary (raised testicle), unilateral and bilateral.
Symptoms
Cryptorchidism is manifested by the absence of one or both testicles in the scrotum. With the development of a one-sided form of the disease, an asymmetry of the scrotum is observed due to its atrophy on the side of the undescended testicle. With bilateral cryptorchidism, both halves of the scrotum are underdeveloped.
Cryptorchidism in men is manifested by dull (pulling, aching) mild pain in the lower abdomen and groin, which increases with physical exertion, straining, sexual arousal and fast walking.
In some cases, when examining the external genital organs at the site of the testicle, a tumor-like formation of a small size is revealed, painful on palpation. In 60% of patients, the testicle is palpated as a sedentary painful formation. When an undescended testicle is localized in the groin, the pubic bone can press on it, which contributes to its injury.
70% of men with bilateral cryptorchidism suffer from infertility.
In the case of the development of false cryptorchidism at a low ambient temperature or muscle tension, the testicle can rise into the inguinal canal and independently return to the scrotum, which is normally developed in such patients.
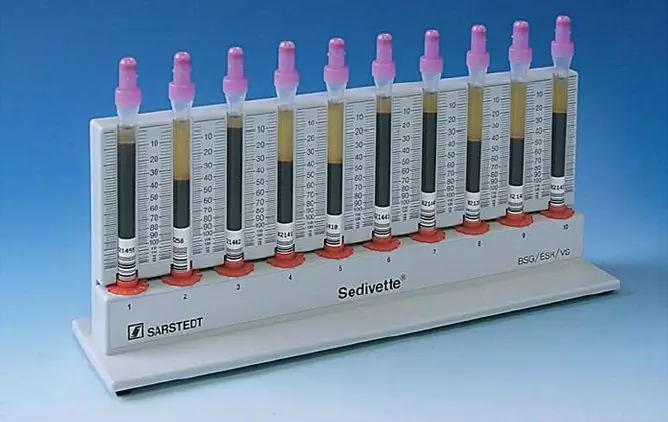
Diagnostics
The diagnosis is made on the basis of an examination; to clarify it, a number of instrumental and laboratory tests are carried out.
The patient is examined in a warm room. In the absence of a testicle in the scrotum, palpate the inguinal canal (downward and medially from the superior anterior iliac spine to the pubic tubercle), the perineum, the suprapubic region, and the femoral canal. When the testicle is localized at the exit of the inguinal canal, an attempt is made to manually bring it down into the scrotum in order to differentiate between true and false cryptorchidism.

Source: o-krohe.ru
For the purpose of differential diagnosis with congenital absence of one (monorchism) or both (anorchism) of the testicles, ultrasound is performed, with insufficient information content - computer or magnetic resonance imaging of the abdominal cavity and pelvic organs.
In some cases, it may be necessary for diagnostic laparoscopy, which, when a testicle is found in the abdominal cavity, is transferred to a therapeutic one: the testicle is brought down into the scrotum.
In the absence of palpable testicles before surgery, it is recommended to conduct a study consisting in the administration of chorionic gonadotropin followed by determination of the concentration of sex hormones in the blood. The absence of an increase in testosterone concentration and an increase in basal levels of luteinizing and follicle-stimulating hormones indicate anorchism.
Treatment
Treatment of false cryptorchidism in children is not required; in adolescence, it usually disappears on its own.
Treatment of true cryptorchidism can be conservative, surgical or combined. Its purpose is to correct the position of the testicles, which is recommended for children in the first two years of life, since otherwise irreversible impairment of spermatogenesis occurs. Until the child reaches nine months, a wait-and-see tactic is chosen, since there is a possibility of independent descent of the testicle into the scrotum.
Drug treatment of cryptorchidism is carried out mainly in the presence of endocrine disorders caused by bilateral cryptorchidism, after determining the level of hormones in the blood. Hormone therapy consists of the use of human chorionic gonadotropin or luteinizing hormone releasing factor. With testicular ectopia, hormonal therapy is ineffective, but in some cases it is used to improve the condition of the tissues before surgery. The greatest effectiveness of drug therapy with hormones is observed in the inguinal form of the disease, in other cases, the effectiveness is estimated at 20-30%.
With the localization of one or both testicles in the abdominal cavity, testicular ectopia, or a combination of this disease with other developmental anomalies, surgical treatment is indicated:
- orchidofuniculolysis - the release of the testicle and spermatic cord from the surrounding tissues;
- orchipexy - bringing down the testicle into the scrotum with its subsequent fixation.
Orchipexy is recommended for children at the age of 12-18 months in one stage.
A two-stage operation for cryptorchidism is performed when the testicle cannot be lowered into the scrotum even with maximum mobilization. During orchipexy, a testicular biopsy is performed in order to exclude gonadal dysgenesis and malignant process. The advantages of performing orchipexy at an early age include preventing infertility, testicular trauma, torsion of the spermatic cord; if necessary, simultaneous correction of oblique inguinal hernias, which accompany cryptorchidism in 90% of cases, can be performed.
With the abdominal form of cryptorchidism, endoscopic reduction of the testicle is used. Laparoscopic orchiectomy is indicated for patients with abdominal unilateral cryptorchidism and short spermatic cord. With a bilateral form of pathology, testicular autotransplantation is performed with its connection to the lower epigastric vessels.

Source: cf.ppt-online.org
If significant morphological changes are detected in the testicle, it is removed (orchiectomy), after which a donor testicle is transplanted or an artificial testicle is implanted for the purpose of cosmetic correction of the defect.
After surgery for cryptorchidism, patients are recommended to be regularly examined in order to timely diagnose possible malignant neoplasms.
Possible complications and consequences
Cryptorchidism can be complicated by impaired spermatogenic function, hormonal disorders, erectile dysfunction, infertility, torsion of the spermatic cord, entrapment of the testicle, and the development of malignant neoplasms.
Forecast
With timely diagnosis and correct treatment, the risk of developing complications of cryptorchidism is significantly reduced. Infertility develops in 70-80% of patients with bilateral cryptorchidism and in 20% of patients with unilateral form of the disease.
Prevention
In order to prevent the development of congenital cryptorchidism in a child, women during pregnancy are advised to:
- prevention and, if necessary, timely treatment of infectious diseases;
- rejection of the irrational use of medicines;
- avoidance of excessive physical and mental stress;
- rejection of bad habits;
- avoidance of occupational hazards;
- balanced diet.
Prevention of acquired cryptorchidism is to prevent injury to the genital organs.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!