- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Hysteroscopy

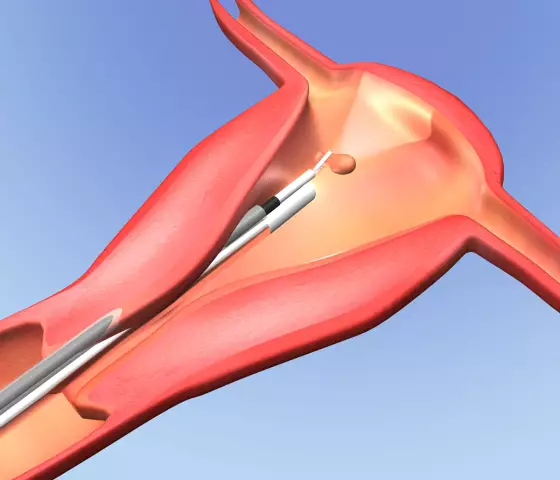
Hysteroscopy is an examination of the uterine cavity using a special endoscopic apparatus (hysteroscope). The term hysteroscopy comes from the words hystero (uterus) and scopy (look, examination). This manipulation is often used in outpatient gynecology, and can be both diagnostic and therapeutic (surgical) in nature. After hysteroscopy, the patient can be immediately sent home, and if the study was diagnostic, then the next day she can go to work.
In gynecological practice, there are many different diagnostic methods (ultrasound of the pelvis, diagnostic curettage, hysterosalpingography), but only hysteroscopy of the uterus allows you to accurately establish the diagnosis, take a biopsy of the material (a piece of tissue of the uterine mucosa) and, if necessary, perform therapeutic measures. Diagnostic hysteroscopy is performed to clarify the diagnosis, medical hysteroscopy is a minimally invasive gynecological intervention, in which it is possible to treat various pathologies from the side of the uterine cavity (for example, removal of a polyp).
Currently, hysteroscopy can be done in a hospital setting and in an antenatal clinic (or a private center). This manipulation must be performed by a specialist who has an appropriate certificate. With diagnostic hysteroscopy, the state of the cervical canal (cervix), the uterine cavity and the mouth of the fallopian tubes are visually examined. If endometrial pathology is detected, it is possible to take a biopsy or perform curettage (curettage of the uterine cavity) in order to send the resulting tissue material for histological examination. Discharge after hysteroscopy is short-lived and does not require special treatment.
Indications for hysteroscopy
Diagnostic hysteroscopy is performed in the following cases:
- Abnormal uterine bleeding;
- Suspected endometriosis of the uterus, submucous myoma, tumor of the uterine body;
- Menstrual irregularities, abnormalities in the development of the uterus;
- Infertility;
- Foreign bodies of the uterine cavity (for example, an intrauterine device, remnants of the ovum after termination of pregnancy);
- Control examination of the uterine cavity after surgery, curettage, miscarriage, and also after treatment with hormonal drugs.
Indications for therapeutic hysteroscopy of the uterus
- Endometrial polyps;
- Endometrial hyperplasia;
- Intrauterine synechiae (adhesions) or intrauterine septum;
- Submucosal myoma;
- Narrowing of the mouth of the fallopian tubes;
- To perform sterilization;
- In order to remove the intrauterine contraceptive (coil).
Contraindications
- Intrauterine pregnancy (progressive). In patients of childbearing age, the possibility of pregnancy should be excluded before performing this procedure (pregnancy test or determination of hCG in urine or blood);
- Acute inflammatory processes of the pelvic organs. Performing hysteroscopy for acute inflammation can lead to the spread of infection, chronic pain in the pelvic area, infertility;
- Profuse uterine bleeding;
- Established advanced cancer of the uterus or cervix. It is technically possible to do hysteroscopy in the oncological process of the small pelvis, but this can lead to the spread of cancer cells into the abdominal cavity;
- Severe condition of the patient as a result of pathology of the cardiovascular, respiratory, nervous systems, with severe liver and kidney diseases.
When can a hysteroscopy be done?
Diagnostic hysteroscopy is performed before the 12th day of the menstrual cycle (usually 7-10 days), in the so-called proliferative phase (when the endometrium thickens under the influence of hormones). In the secretory phase (the second half of the menstrual cycle), this examination is not carried out, since during this period the state of the endometrium can be assessed incorrectly.

In emergency cases and while taking hormonal contraceptives, hysteroscopy can be done on any day of the cycle.
Anesthesia
Most patients experience pain during hysteroscopy, which can interfere with a full examination of the uterine cavity. Recently, preference has been given to hysteroscopy of the uterus under local anesthesia, but it is possible to perform manipulations under general anesthesia (intravenous).
Technique for hysteroscopy
When performing hysteroscopy, the expansion of the cervical canal is not required, since the hysteroscope is thin enough to pass into the uterine cavity. During the procedure, a sterile fluid is injected in order to make all the walls of the uterus accessible for inspection. The doctor can visually inspect the uterine cavity, record the procedure on video. If a pathology is detected, a piece of tissue is taken for a biopsy, or other manipulations are performed. Usually the hysteroscopy procedure lasts 10-30 minutes.
Complications
Complications after hysteroscopy are rare (less than 1%). Nevertheless, the procedure is invasive, therefore, negative consequences are possible in the form of: perforation of the uterine wall, rupture of the cervix, bleeding, exacerbation of a chronic inflammatory process.
Discharge after hysteroscopy
After hysteroscopy, there may be bleeding from the genital tract. Scanty spotting after hysteroscopy is almost always present for several days (usually 2-3). Moderate pain in the lower abdomen in the form of spasms is also possible (usually within 1-2 days).
With discharge after hysteroscopy, tampons should not be used in order to prevent the inflammatory process. Also, the doctor will recommend refraining from sexual intercourse for several days (after diagnostic hysteroscopy) or 2-3 weeks (after treatment).
Found a mistake in the text? Select it and press Ctrl + Enter.