- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Hepatosis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
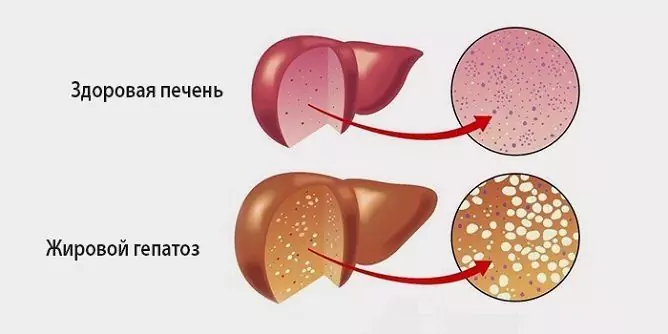
Hepatosis is a group of non-inflammatory liver diseases, the development of which is caused by hereditary or exogenous factors. They are characterized by atrophy of hepatocytes and impaired metabolic processes in the liver.

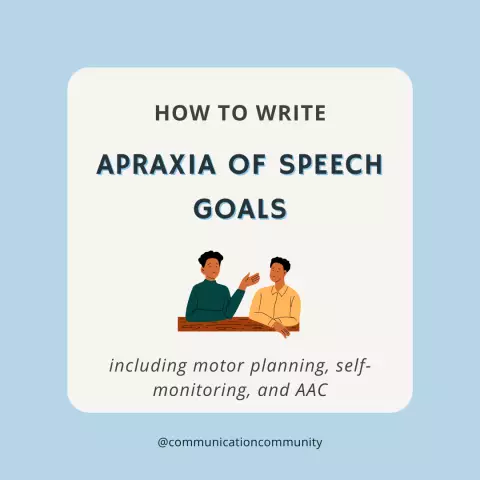
Dystrophic changes in the liver with fatty hepatosis
Causes and risk factors
There are many reasons that can cause the development of hepatosis. They are divided into two groups: hereditary and external (exogenous). Hepatitis is associated with genetically determined disorders of the metabolism of bilirubin and bile acids in the liver. Pathologies of this kind include:
- Rotor syndrome;
- Dabin-Johnson syndrome;
- Lucy-Driscoll syndrome;
- Crigler-Nayar syndrome;
- Gilbert's disease.
The pathogenesis of these diseases is due to a hereditary defect in the synthesis of enzymes responsible for the binding, transport and release of bilirubin.
External causes of the development of hepatosis include diseases that have a toxic effect on the liver (obesity, diabetes mellitus, thyroid pathology), alcohol abuse, poisoning (poisonous mushrooms, some drugs, organophosphate poisons).

Diabetes mellitus in combination with obesity leads to fatty liver hepatosis
Forms of the disease
Depending on the reasons that caused them, hepatosis is divided into several types:
- Alcoholic fatty hepatosis. After viral hepatitis, it is considered the second most important liver disease. The severity of its manifestations is determined by the duration of the consumption of alcoholic beverages and their quantity, while the quality has practically no effect on the course of the disease. A feature of this form is that the rejection of alcohol can lead to regression of clinical manifestations of hepatosis and morphological changes in the liver.
- Non-alcoholic fatty hepatosis. In pathogenesis, the main role belongs to the necrosis (death) of hepatocytes followed by their replacement with adipose (adipose) tissue. The disease is widespread - among all chronic liver pathologies, it accounts for 10%. Most often, non-alcoholic fatty hepatosis of the liver is asymptomatic and only in rare cases causes the development of portal hypertension, liver failure, cirrhosis.
- Toxic hepatosis. It occurs as a result of exposure to the body of certain chemical compounds (organophosphorus poisons, solvents, salts of heavy metals) or toxins of natural origin (pale toadstool, lines). Toxic hepatosis has different variants of the clinical course, and also differ in morphological changes in the liver tissue. The hepatotoxic effect of poisons increases against the background of alcoholism, severe general diseases, protein starvation, viral hepatitis.
- Hereditary hepatosis. It is observed in 2-5% of the population. In most cases, it proceeds favorably and does not cause pronounced morphological changes in the liver cells, provided that patients comply with the principles of proper nutrition and a healthy lifestyle. The most common form of hereditary hepatosis is Gilbert's disease (unconjugated non-hemolytic hereditary hyperbilirubinemia), which is usually diagnosed in young and middle-aged men. External factors (the use of anabolic steroids and a number of antibiotics, alcohol consumption, stress, significant physical activity, severe infectious diseases, operations, a low-calorie diet) can provoke the development of a crisis in hereditary forms of hepatosis.

The form of hepatosis is due to the cause that caused the disease
Symptoms
The clinical pictures of different forms of hepatosis differ.
With toxic hepatosis, the symptoms are pronounced:
- high body temperature;
- icteric staining of the sclera and skin;
- dyspepsia (nausea, bitterness in the mouth, belching, bloating, stool disturbances);
- pain in the epigastric region or right hypochondrium;
- significant darkening of urine.
Symptoms of fatty hepatosis are much less pronounced:
- occasional jaundice;
- diarrhea;
- occasionally nausea;
- intermittent pulling or aching pain in the right upper quadrant of the abdomen.
The clinical picture of Gilbert's disease is characterized by:
- dull aching pains in the right side of the abdomen;
- moderate hepatomegaly.
In the interictal period, these symptoms are detected in about 75% of patients, and during an attack - in all; in addition, jaundice develops.

With hepatosis, jaundice develops
A rare form of hepatosis is Crigler-Nayyar syndrome. Its first symptoms are already noticeable during the neonatal period. The syndrome has two types of clinical course. The first is characterized by high hyperbilirubinemia, which leads to rapid toxic damage to the central nervous system and the death of the child. The second type is more favorable and is manifested by moderate jaundice.
Very rare forms of hereditary hepatosis:
- Rotor syndrome - manifested by yellowness of the sclera, which can be aggravated by taking certain medications;
- Dabin-Johnson syndrome - characterized by impaired bile secretion, icteric staining of the sclera, aggravated by hormonal contraception;
- Lucy-Driscoll syndrome - the appearance of jaundice is associated with breastfeeding, transferring the baby to artificial feeding eliminates the clinical manifestations of liver pathology.
Diagnostics
Diagnosis of hepatosis is carried out by excluding other liver diseases. A laboratory blood test is prescribed for antibodies to viral hepatitis or antigens. To assess the functional abilities of the liver, a biochemical blood test, a coagulogram is performed, urine and feces are examined for the content of bile pigments.

Ultrasound of the liver reveals structural and morphological changes in the organ
An informative diagnostic method at the primary stage is considered to be ultrasound, which makes it possible to identify and assess structural and morphological changes in the liver tissue. For a more detailed study of the revealed changes, multispiral computed tomography (MSCT) of the abdominal organs or magnetic resonance imaging of the liver are performed. If changes in the liver of a non-inflammatory nature and fatty deposits are detected, a puncture biopsy is recommended, followed by a histological analysis of the obtained tissue sample.
If you suspect Gilbert's disease, the following provocative tests are performed:
- Test with nicotinic acid. Before the start of the study, the content of bilirubin in the blood is determined. After that, nicotinic acid is injected intravenously. After 5 hours, repeat determination of bilirubin in blood serum. Its increase by more than 25% confirms the diagnosis.
- Sample with a low-calorie diet. The initial level of bilirubin in the blood serum is determined, then a diet with a significant restriction of calories is prescribed for 48 hours, after which the blood is again examined for the content of bilirubin. Confirmation of the diagnosis is an increase in the concentration of bilirubin by more than 50%.
Treatment
In most cases, hepatosis is treated on an outpatient basis. Only with a significantly pronounced crisis may there be a need for hospitalization of the patient in the gastroenterology department.
For non-alcoholic fatty hepatosis, diet and exercise therapy are recommended. In the diet, fats and carbohydrates are limited and the proportion of proteins is increased. In combination with moderate physical activity, such nutrition helps to gradually reduce body fat, including in the liver. The use of alcoholic beverages should be completely abandoned - this is the main condition for effective treatment. Drug therapy for non-alcoholic fatty hepatosis is based on the use of hepatoprotectors and membrane stabilizers.

An indispensable condition for the successful treatment of hepatosis is a ban on alcohol
With hereditary hepatosis, patients are advised to adhere to a healthy lifestyle and proper nutrition, avoid significant physical exertion. Vitamin therapy courses are shown every year in autumn and spring.
With Gilbert's disease, patients do not need pharmacotherapy aimed at lowering serum bilirubin levels. In most cases, by age 50, hyperbilirubinemia resolves on its own.
Treatment of type I Crigler-Nayyar syndrome consists of replacement blood transfusion and phototherapy. In type II, bilirubin-lowering drugs and moderate phototherapy are prescribed.
Treatment of Lucy-Driscoll syndrome consists in the abolition of breastfeeding and the transfer of the child to artificial formula nutrition.
Possible complications and consequences
In most cases, hepatosis is not accompanied by the development of serious complications. The exception is type I of the Crigler-Nayyar syndrome - children suffering from it die in the first years of life.
Forecast
The forecast is favorable. With the elimination of the causative agent, hepatosis can proceed for a long time, without causing serious morphological and structural changes in the liver.
Prevention
Prevention of acquired hepatosis includes the following measures:
- avoiding alcohol abuse;
- balanced diet;
- maintaining a healthy lifestyle;
- refusal to take medications without a doctor's prescription;
- careful handling of toxic substances.
Prevention of congenital hepatosis has not been developed. If one of the spouses suffers from this pathology or it was observed in one of the relatives, then at the stage of planning pregnancy, the married couple is recommended to receive medical genetic counseling.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!