- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Hemarthrosis of the knee joint
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms of hemarthrosis of the knee joint
- Diagnostics
- Treatment of hemarthrosis of the knee joint
- Potential consequences and complications
- Forecast
- Prevention
Hemarthrosis of the knee joint is an outpouring of blood into the articular cavity, which develops as a result of rupture of blood vessels supplying the joint with blood.

Signs of hemarthrosis of the knee joint
Causes and risk factors
The main reason for the development of hemarthrosis of the knee joint is its traumatic injury (bruises, rupture of the meniscus, capsule, subluxation, dislocation, fracture).
Other reasons leading to the accumulation of blood in the articular cavity can be:
- condition after surgery on the knee joint (arthroplasty, stitching of the cruciate ligaments, removal of the meniscus, osteosynthesis of the condyles of the thigh or tibia, etc.);
- blood clotting disorders (taking anticoagulants in high doses, hemophilia);
- hemorrhagic fevers;
- malignant tumors in the knee joint;
- diseases of the blood vessels, leading to increased fragility or permeability of their walls.

The most common cause of hemarthrosis is a knee injury
The medical literature describes cases of the development of hemarthrosis of the knee joint in patients with deforming osteoarthritis of the knee, accompanied by degenerative-dystrophic changes in the external meniscus.
Often, hemarthrosis of the knee joint develops as a result of a sports injury or road traffic accidents. In the latter case, it is usually combined with other injuries (polytrauma).
The disease is typical for patients suffering from hemorrhagic diathesis and some other diseases in which vascular permeability or blood clotting is impaired (for example, scurvy or hemophilia). In such patients, bleeding into the articular cavity can result in a very insignificant effect, which often goes unnoticed by the patient himself. Hemorrhage can occur anywhere in the body, but the knee joint is more exposed to daily stress than others, and therefore is especially vulnerable.
The poured out blood increases the pressure in the articular cavity, provokes pain, makes it difficult to move in the joint. In addition, the blood that has entered the cavity of the knee joint leads to the development of aseptic inflammation, which has a destructive effect on the hyaline cartilage, which covers the articular surfaces of the bones. After a while, the poured blood coagulates, forming blood clots. Subsequently, they are impregnated with calcium salts and sprout with connective tissue fibers. As a result, adhesions are formed in the articular cavity, initially loose and soft, and then turning into rough ones.
The spilled blood is a breeding ground for pathogenic microorganisms, therefore hemarthrosis of the knee joint is often complicated by the addition of a secondary purulent infection.
Forms of the disease
Depending on the cause, there are traumatic and non-traumatic hemarthrosis of the knee joint.
Symptoms of hemarthrosis of the knee joint
The clinical symptoms of hemarthrosis of the knee joint are determined by the volume of blood flowing out. Depending on this, there are three degrees of severity of the disease:
- Lightweight. The volume of blood in the articular cavity does not exceed 15-20 ml. In the clinical picture, the manifestations of the main injury come to the fore, as a rule, it is a contusion of the knee joint. There is no feeling of fullness in the affected joint, the pain is slightly expressed. The patient can lean on the injured leg.
- Medium severity. Occurs when pouring into the cavity of the knee joint from 20 to 100 ml of blood. The contours of the joint are smoothed, it increases in volume, taking on a spherical shape. On palpation, fluctuation is well defined (a sign of the presence of fluid in a closed cavity). A significant amount of accumulated blood is accompanied by the appearance of a noticeable bulging on the sides of the patella. The functions of the knee are limited, movement in it is sharply painful.
- Heavy. The volume of blood flowed out exceeds 100 ml. The soft tissues surrounding the affected knee joint become tense and tight, and their temperature rises. The skin over the joint becomes bluish in color. Joint movements are impossible.

What does hemarthrosis of the knee joint look like at different stages
With significant hemarthrosis of the knee joint, the blood begins to thin after a few days, which is accompanied by a softening of the swelling of the affected joint. When the position of the body changes, the swellings on the sides go down. Sometimes, during palpation, large blood clots are determined.
Diagnostics
Diagnosis of hemarthrosis of the knee joint is carried out on the basis of characteristic clinical signs, anamnesis data and the results of instrumental examination.
In hemarthrosis, an X-ray of the knee joint is performed in two projections, which makes it possible to identify possible damage to the bones. If there is a suspicion of cartilage damage or ligament rupture, arthroscopy, computed tomography or magnetic resonance imaging of the knee joint is performed.

X-rays are taken to diagnose hemarthrosis of the knee
If hemarthrosis of the knee joint occurs under the influence of a minor injury, it can be assumed that the patient has blood coagulation disorders. In this case, a consultation with a hematologist and a number of laboratory tests are necessary to assess the state of the blood coagulation system:
- thrombin time;
- the concentration of fibrinogen in the blood;
- determination of the clotting time of capillary and venous blood;
- determination of the number of blood coagulation factors;
- activated partial thromboplastin time;
- international normalized attitude;
- prothrombin index;
- platelet count.
Treatment of hemarthrosis of the knee joint
If hemartosis of the knee joint is suspected, the victim should be taken to a traumatologist. At the prehospital stage, the affected limb is placed on a flat horizontal surface, and a cotton-gauze roller or a small pad is placed under the knee joint. A bag of ice wrapped in a towel or a heating pad with cold water is applied to the joint from above.
The choice of a method for treating hemarthrosis of the knee joint is determined by the severity of the disease.
With hemarthrosis of the first degree, there are no indications for performing intra-articular puncture, since the volume of blood in the articular cavity is minimal. The affected joint is immobilized with a plaster cast, giving the limb an elevated position. The duration of immobilization depends on the nature of the primary injury. During the first 24-48 hours from the moment of injury, cold is applied to the knee joint, and then UHF is prescribed to accelerate the resorption of the intra-articular hematoma.

Intra-articular puncture for hemarthrosis of the knee joint is performed when the volume of blood in the joint cavity exceeds 25-35 ml
In cases where the volume of blood poured into the joint cavity exceeds 25-35 ml, it is removed to prevent the development of complications. For this, intra-articular puncture of the knee joint is performed under local anesthesia. After removing the blood, the articular cavity is washed with a solution of novocaine, and then triamcinolone or hydrocortisone is injected into it. Then the joint is tightly bandaged and immobilized with a plaster cast in order to limit mobility. After that, the patient is recommended to bed rest with giving the limb an elevated position, walking only on crutches. In some cases, blood re-accumulates in the knee joint, which necessitates repeated punctures.
In cases where hemarthrosis of the knee joint develops against a background of blood diseases, the standard treatment is supplemented by the administration of antihemophilic globulin, transfusion of fresh frozen plasma.
With the development of synovitis, antibacterial drugs are prescribed, taking into account the sensitivity of the microflora to them. Antibiotics are injected into the cavity of the affected joint during punctures and used systemically.
If, during the diagnosis, loose bone or cartilage fragments are detected in the joint capsule, as well as in the presence of serious injuries to the ligamentous apparatus or rupture of the meniscus, treatment is carried out by arthroscopy.
In the recovery period, physiotherapy is indicated (ultrasound, ultra-high-frequency currents, laser radiation, sinusoidal simulated currents, electrophoresis). After removing the plaster, the damaged knee joint is gradually developed with the help of massage and physiotherapy exercises. The rehabilitation period for hemarthrosis of the knee joint lasts at least six months. A knee pad must be worn during this period.

In the recovery period, physiotherapy is indicated.
Potential consequences and complications
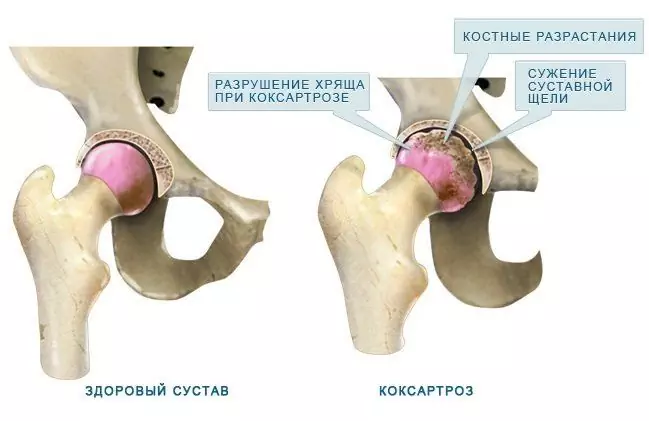
When red blood cells are destroyed, hemosiderin is formed, which negatively affects the hyaline cartilage and ligamentous apparatus, as a result of which they lose elasticity. The surface of the cartilage becomes covered with cracks and becomes thinner, which over time leads to the development of deforming osteoarthritis of the knee joint.
The decomposition products of blood have high biological activity and can cause inflammation of the synovial membrane - synovitis. In turn, synovitis causes the development of aseptic arthritis.
Another common complication of knee hemarthrosis is purulent arthritis. Its development is caused by the penetration into the articular cavity with accumulated blood of pyogenic microorganisms from any other focus of chronic infection in the body by hematogenous or lymphogenous route.
Forecast
With timely treatment of traumatic hemarthrosis of the knee joint, the prognosis is favorable.
Hemarthrosis, which has arisen against the background of severe injuries of the knee joint, or frequent relapses of hemorrhages in the articular cavity, caused by hemorrhagic diathesis, hemophilia, often lead to the development of complications.
Prevention
Prevention of the occurrence of hemarthrosis of the knee joint is reduced to the prevention of its injuries in everyday life and at work. When practicing traumatic sports (hockey, handball, etc.), protective equipment must be worn.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!