- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Portal hypertension syndrome
The content of the article:
- Etiology and pathogenesis
- Classification
- Stages
- Portal hypertension symptoms
- Diagnostics
- Treatment of portal hypertension
- Forecast
- Video
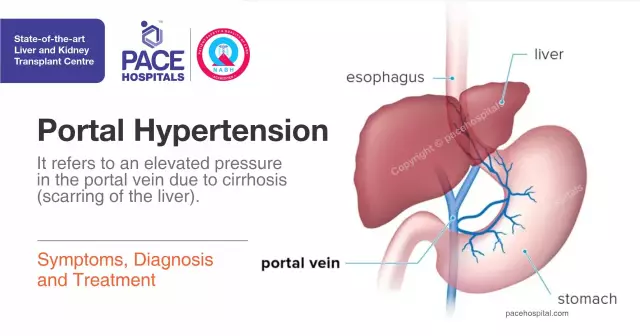
Portal hypertension (portal hypertension syndrome) is a pathological condition that is caused by a significant increase in pressure in the portal vein system, one of the main veins of the liver. There are many reasons for this, but the most common are cirrhosis of the liver, vascular pathologies of the liver, decompensated heart failure, much less often schistosomiasis. Since the liver is the organ with the most massive blood circulation (the portal vein system and the liver can deposit up to half of the total blood volume), congestion inside this parenchymal organ and nearby tissues is fraught with consequences for the whole organism.

Increased pressure in the portal vein system creates prerequisites for the development of life-threatening conditions
The disease is also dangerous with formidable complications in the form of hepatic encephalopathy, circulatory disorders, endogenous intoxication, varicose veins of the esophagus, threatening internal bleeding, impaired blood outflow from the intestine - this is only a small part of what can result from an increase in pressure in the portal vein. It is positive that in most cases the pathology develops slowly and is chronic, and doctors have enough time to provide assistance.
Etiology and pathogenesis
What is portal hypertension? To understand the process of the formation of pathology, you should know that the portal vein is one of the largest and most important veins in the body. It is connected by anastomoses with the vena cava, dense capillary network of the liver, hepatic veins. An increase in pressure in it leads to an increase in pressure in all veins of the abdominal cavity, saphenous veins, in the vessels of the spleen (hypertension is usually accompanied by splenomegaly - an enlargement of the spleen), the appearance of non-inflammatory effusion in the abdominal cavity due to the prevalence of hydrodynamic blood pressure over oncotic pressure, which must hold water in the vascular bed.
The main etiological factors that lead to hypertension in the portal vein basin:
- Hepatitis of any etiology - lead to massive inflammation of the liver parenchyma, the development of adhesions, a decrease in the area of effective passage of blood through the hepatic lobules. If the inflammation progresses, necrosis of hepatocytes is observed, and in their place is formed connective tissue that is incapable of circulating and acting only structurally (but not functionally) - cirrhosis of the liver.
- Liver cirrhosis - can be caused by viruses, bacteria, invasions, alcoholic cirrhosis is common. When most of the parenchyma is replaced by fibrous tissue, the liver stops functioning at full strength and blood flow does not decrease. The dense structure does not allow the required volume to pass through, and the pressure in the portal vein increases.
- Fatty hepatosis, or fatty degeneration of the liver - the mechanism of development is similar to cirrhosis, with the only difference that instead of fibrous tissue, the inner part of the organ is replaced with fatty tissue. It also reduces the effective organ area and impairs the passage of blood through the acini.
- Diseases that reduce the lumen of the portal vein - thromboembolic conditions, congenital vascular anomalies, tumors that narrow the lumen of the vein.
- Portal liver fibrosis.
The disease develops in several stages, of which an increase in pressure inside the liver itself, an increase in vascular resistance in the sinusoids and terminal venules, and hepatic lobules play a critical role. An important role is played by biochemical damage to the liver by decay and stagnation products, biologically active substances of venous blood, in particular, disintegrating hemoglobin, as well as edema of hepatocytes (liver cells).
The body is able to effectively compensate for a sluggish pathological process for some time, when blood circulation is performed along bypass routes - shunts or collaterals. But then the overflow of portocaval and portosystemic anastomoses leads to varicose swelling of these veins and other vessels in their basin, ascites, and bleeding. Due to the fact that blood circulation bypasses the liver, and it is the main organ that purifies the blood from foreign substances (as well as from internal metabolic products, xenobiotics - alcohol, drugs, etc.), all these substances enter into free circulation, and then into target organs, in particular, the brain. Thus, the intoxication of the body is increasing.
Disorders that affect protein metabolism are also dangerous, although they are not primary - the liver synthesizes the largest amount of proteins in the body, therefore, with its diseases, the level of blood proteins falls, and with them oncotic pressure, nonspecific immunity, the ability of blood to coagulate hemostasis (clotting). Separately, it is worth highlighting an increase in the spleen, often associated with an increase in its function (hypersplenism), which is fraught with anemia and thrombocytopenia.
Classification
The generally accepted classification takes into account conditions that can result in hypertension in the portal vein system:
- Suprahepatic - caused by thrombosis (obstruction) of the splenic or portal vein, which leads to an accumulation of blood in the portal vein through the nearest anastomosis. This type also includes congenital pathologies, such as atherovenous fistula.
- Hepatic - in relation to the hepatic sinus, there are three types: presinusoidal, sinusoidal (cirrhotic) and postsinusoidal (due to hepatic veno-occlusive disease). With this form of the disease, the liver itself is the cause of stagnation.
- Extrahepatic - more common in children in the context of Budd-Chiari syndrome, manifested by thrombosis of the hepatic vein, obliterating endophlebitis of the hepatic veins, or cardiac pathology in the form of an increase in hydrodynamic pressure in its chambers and a decrease in the effective volume of the heart.
Stages
The clinic distinguishes 4 stages of pathology, depending on the severity of manifestations:
- the initial, it is also the functional stage - characterized by a slight increase in pressure in the portal vein, which may decrease after a while; target organ damage is absent;
- grade 1, moderate or compensated - at this time the body is still coping with the blood flow using roundabout collaterals. The veins of the esophagus are slightly dilated, ascites is absent, slight splenomegaly is possible;
- degree 2, pronounced - characterized by splenomegaly, an abundance of clinical signs, in particular, edema syndrome, ascites, hemorrhages;
- grade 3, complicated - hypertension is complemented by bleeding from the veins of the esophagus, stomach, rectum, hemorrhoidal veins; severe anemia is possible. It is a terminal state.
Portal hypertension symptoms
Disease symptoms vary with patient-specific compensation, absolute portal pressure, and complications.
The first manifestations of pathology are usually digestive disorders, flatulence, loose stools, pain in the left and right epigastric region, a feeling of bloating and fullness of the abdomen. Characterized by the so-called hepatic weakness, fatigue, drowsiness.
Later, splenomegaly is detected, which is determined by palpation. An enlarged spleen can cause pain, press on surrounding organs, overfulfill its function, destroying platelets and red blood cells at a high rate and thereby causing anemia and thrombocytopenia (therefore, it is necessary to prescribe a general and biochemical blood test). An insufficient number of shaped elements indicates the progression of the process.

"Medusa's head" is one of the characteristic signs of hypertension in the portal vein system
An important diagnostic criterion is the so-called head of a jellyfish - an increase in the saphenous veins of the anterior abdominal wall, contrasting of the sinuous venous pattern of the anterior abdominal wall. Often this symptom is accompanied by ascites, which can be determined using the fluctuation method, when the doctor shakes the abdominal wall, on one side, and with the other hand feels a wave, the movement of fluid. Outwardly, ascites is manifested by an increase in the abdomen, acquiring a rounded shape.
A common symptom of portal hypertension is internal bleeding that occurs suddenly for no apparent reason. It is due to bleeding that patients often seek medical help for the first time. It can be bleeding from the veins of the esophagus (blood is red, light), stomach (blood in contact with hydrochloric acid of gastric juice acquires the color of coffee grounds), hemorrhoids. This condition requires surgical intervention.
The patient has general dystrophy (a characteristic appearance of such patients is a disproportionately enlarged abdomen due to ascites against the background of thin arms and legs), a decrease in muscle mass, and muscle weakness. Toxic brain damage leads to encephalopathy - the patient has poor articulation, answers questions inappropriately, does not remember well, thinks about simple questions for a long time, often does not understand the meaning of what has been said.
Diagnostics
Diagnosis of the disease is multi-stage, in the absence of severe complications, together with treatment, it is carried out in the therapeutic department, if any, in surgery. First, the doctor conducts an examination, analyzes the condition of the skin, saphenous veins of the abdomen, a general view of its front wall. Then he makes palpation and percussion - he looks for free fluid in the abdominal cavity, palpates the surface and edge of the liver, spleen. With this pathology, they are hard, dense, sharp, sometimes painful. After physical examination, they proceed to instrumental and laboratory examinations.
X-ray with contrast is used - this way you can assess the state of hepatic blood flow. In some cases, they resort to liver scintigraphy, this method is similar to radiography, only a radiopharmaceutical acts as a contrast.
An informative method is ultrasound of the abdominal cavity, which allows you to assess the size, structure, echogenicity of the liver, spleen and nearby vessels. An ultrasound sign of hypertension is an increase in the diameter of the hepatic veins, portal and vena cava. If you combine ultrasound with Doppler ultrasound, it is possible to thoroughly assess the blood flow and hemodynamic conditions in specific vessels.
Mandatory studies are FGDS (fibrograstroduodenoscopy), sigmoidoscopy. Endoscopic methods allow assessing the degree of damage to the veins of internal organs, their swelling, and the risk of bleeding.
Laboratory examination includes, in addition to a clinical blood test, the study of coagulogram, markers of hepatitis, enzymes ALT, AST, their ratio, LDH of various fractions, serum immunoglobulins.
Treatment of portal hypertension
Treatment begins with the use of pharmacological agents, the action of which is aimed at removing free fluid from the body, expanding the lumen of blood vessels, and improving hemodynamics. For this purpose, beta-blockers (Atenolol, Nebivalol), diuretics (Furosemide, Lasix), ACE inhibitors (Captopril, Lisinopril), glycosaminoglycans are prescribed. For bleeding, Telipressin or Vasopressin is prescribed.
It is critically important to treat the underlying condition that caused the hypertension.
In some cases, the therapeutic effect is insufficient and surgery is necessary. As a rule, surgical intervention in both adults and children is performed by the laparoscopic method.
Attention! Photo of shocking content.
Click on the link to view.
In order to stop internal bleeding, they resort to endoscopic sclerotherapy, in which a drug is injected into the vessel, causing the vascular walls to stick together. This manipulation has medical reviews indicating its high efficiency. Also, in case of bleeding, vessel ligation is performed, that is, ligation of the bleeding vein.
With severe ascites, laparocentesis is performed - removal of free fluid from the abdominal cavity.
The main method of surgical treatment for portal hypertension is the creation of artificial shunts to reduce the pressure in the portal vein. Perhaps the imposition of artificial portocaval or mesentericocaval anastomoses, through which the blood will go around. Unfortunately, the functionality of the liver cannot be restored by any of the currently existing methods, therefore all operations are palliative in nature.
Forecast
The average lifespan of patients with this pathology is 10-15 years after an operation to impose artificial anastomoses. This is a fairly high figure considering the scale of the damage. This period can be extended by adequate prevention of complications, supportive therapy, and regular medical examinations.
Clinical guidelines are to normalize the daily regimen and diet. It is necessary to limit the use of salt and other foods that increase blood pressure. It is also important to monitor the volume of fluid consumed, not to exceed the recommended volume (set by the doctor on an individual basis). Heavy physical activity is strictly prohibited.
The lethal factor is most often internal bleeding; this complication accounts for more than 50% of deaths in this pathology.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.