- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Arrhythmogenic right ventricular dysplasia
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Arrhythmogenic right ventricular dysplasia (arrhythmogenic right ventricular cardiomyopathy) is a rare disorder that is thought to be based on genetic causes. It is characterized by structural changes in the structure of the wall of the right ventricle, consisting in the replacement of cardiomyocytes with fibrous-adipose tissue, and the development of arrhythmia.
The incidence of arrhythmogenic right ventricular dysplasia (ARVD) is 1 to 6 cases per 10,000 population. It occurs four times more often in men than in women.
After it was found that there is a relationship between sudden cardiac death syndrome and arrhythmogenic right ventricular dysplasia, the interest of scientists in this disease has increased dramatically. The results of scientific studies have shown that in children and adolescents under 20 years of age who died from cardiovascular pathology, in every fourth case in the myocardium there were histological changes characteristic of ARVD.

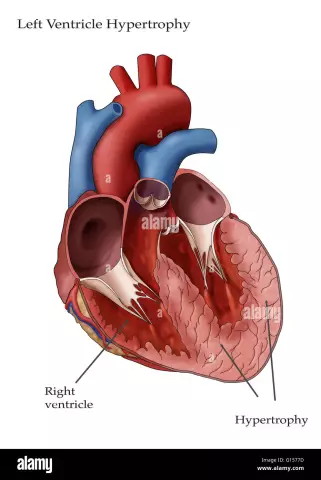
Replacement of cardiomyocytes with fibrous-adipose tissue is a sign of arrhythmogenic right ventricular dysplasia
Causes and risk factors
There is no common point of view among the scientific community regarding the causes underlying the development of arrhythmogenic right ventricular dysplasia. This is largely due to the variety of its clinical forms. It is likely that the pathology includes not one, but several diseases with similar symptoms, but different etiology. However, most researchers believe that genetic mutations lead to the development of ARVD.
Genetic studies in patients with arrhythmogenic right ventricular dysplasia have shown that the latter have abnormalities of genes located in the 12th, 14th, 17th and 18th chromosomes. These genes are responsible for the synthesis of specific proteins in the myocardium. Changes in the structure of proteins lead to a decrease in the resistance of myocardial cells to damaging effects. This becomes the reason for the replacement of myocardial cells with adipose tissue over time. The structural anomaly of desmoplakin causes a disturbance in the passage of a nerve impulse through the myocardium, which leads to the development of arrhythmia.
In addition, there is a form of arrhythmogenic right ventricular dysplasia, in which an inflammatory process occurs in the myocardium of the right ventricle, which causes the replacement of its cells by fibrous tissue. This form is characterized by a severe course and the transition of the pathological process to other parts of the heart. Presumably, it is also caused by genetic mutations that reduce the resistance of the myocardium to viral damage.
Gene mutations underlying the pathological mechanism of development of arrhythmogenic right ventricular dysplasia are inherited in an autosomal dominant manner with low penetrance, not exceeding 30-50%. This means that even if a child inherits an altered gene from one of the parents, then the probability of a clinical picture of the disease in him is no more than 50%.

Scientists suggest that the main cause of ARVD development is a genetic mutation
There is only one form of ARVD inherited in an autosomal recessive manner with high penetrance (over 90%) - Naxos disease. It is extremely rare: to date, only 25 cases of this disease are known.
Forms of the disease
Depending on the features of inheritance and the clinical course of arrhythmogenic right ventricular dysplasia, the following forms are distinguished:
- Reference or pure form.
- Naxos disease. It manifests itself as malignant arrhythmia, which becomes the cause of death of patients in childhood.
- Venetian cardiomyopathy. The wall of the left ventricle is sometimes involved in the pathological process. Most patients die in childhood.
- Smoke disease. Leads to sudden cardiac death in adolescent boys.
- Tachycardia without manifestations of heart failure or extrasystoles with a focus of pathological excitement in the right ventricle.
- Extrasystole with a focus of excitation in the right ventricle and the presence of signs of an inflammatory process in the myocardium. It is often fatal.
- Uhl's anomaly. An extremely rare form of ARVD, in which almost all myocardial cells of the right stomach are gradually replaced by fibrous-adipose tissue, which leads to the development of progressive cardiovascular failure and death.
- Nonarrhythmic form. In most cases, it is asymptomatic, most often it becomes the cause of sudden cardiac death.
Symptoms
Variants of the clinical course of arrhythmogenic right ventricular dysplasia can vary widely.
The asymptomatic form usually does not manifest itself during the patient's life. Even with electrocardiography, no changes can be detected.
With an arrhythmic form of ARVD, patients develop tachyarrhythmias, ventricular extrasystoles, which are diagnosed during an ECG. Subjective symptoms are usually absent.

ARVD may not manifest itself in any way or is characterized by pain in the region of the heart and tachyarrhythmia
The pronounced clinical form of arrhythmogenic right ventricular dysplasia is characterized by the following features:
- tachyarrhythmia;
- pain in the region of the heart;
- dizziness.
The most severe course is observed with the development of right ventricular heart failure, which is characterized by the appearance of venous stasis of blood, edema, including cavity.
Diagnostics
To diagnose arrhythmogenic right ventricular dysplasia, a detailed cardiological examination is performed, including:
- echocardiography;
- electrocardiography;
- radiopaque ventriculography;
- magnetic resonance imaging with gadolinium contrast.
If necessary, a puncture biopsy of the myocardium is performed, followed by a histological examination of the biopsy.

Arrhythmogenic right ventricular dysplasia: ECG results
An important diagnostic sign, indicating the presence of possible arrhythmogenic right ventricular dysplasia, is an indication of the family nature of the disease, as well as cases of sudden death of relatives.
Treatment
Conservative treatment of arrhythmogenic right ventricular dysplasia includes the appointment of antiarrhythmic drugs. If drug therapy is ineffective, there are indications for the implantation of a pacemaker or cardioverter-defibrillator. In case of right ventricular heart failure, the patient is prescribed ACE inhibitors.
Surgical methods of treatment of arrhythmogenic dysplasia of the right ventricle are also used, consisting in excision of pathological foci of excitation with subsequent suturing of the myocardium. The condition of patients in the first time after surgery improves significantly, however, after several years, 30-40% of operated patients have a relapse of the disease.

Pacemaker implantation is indicated in case of ineffectiveness of ARVD drug therapy
With severe heart failure, the only way to save a patient's life is with a heart transplant.
Possible complications and consequences
Arrhythmogenic right ventricular dysplasia can be complicated by fulminant myocarditis, leading to rapid death of patients.
Forecast
Since the disease is highly variable, the prognosis is uncertain. In some patients, from the onset of the first symptoms to the development of severe heart failure, it takes 1-2 months, while in others, arrhythmogenic right ventricular dysplasia can go on for life with minimal or no manifestations.
Timely started and regularly administered antiarrhythmic therapy reduces the likelihood of death by 35%. The best results are provided by complex treatment, including drug therapy of arrhythmia and implantation of a pacemaker, in which ventricular fibrillation is practically excluded.
The development of heart failure significantly worsens the prognosis.
Prevention
There are no preventive measures aimed at preventing the occurrence of arrhythmogenic right ventricular dysplasia, since the disease is of a genetic nature. If there have been cases of this disease in the family, then at the stage of pregnancy planning, spouses are advised to consult with a geneticist.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!