- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Meningoencephalitis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
-
Symptoms
- Tick-borne meningoencephalitis
- Herpetic meningoencephalitis
- Rabies meningoencephalitis
-
Meningococcal meningoencephalitis
- Amebic meningoencephalitis
- Anti-NMDA receptor meningoencephalitis
- Features of the course of meningoencephalitis in children
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
- Video
Meningoencephalitis is an inflammatory process that affects the membranes and substance of the brain. Despite the fact that the brain is protected by the blood-brain barrier, which prevents the penetration of most foreign and toxic substances into it, some pathogens are still able to pass through it and cause inflammation. Meningoencephalitis, given the importance of the anatomical area it affects, is a life-threatening disease.

Meningoencephalitis is characterized primarily by headache and various disorders of the nervous system
Causes and risk factors
Meningoencephalitis is more likely to be infectious, but it can also be toxic and autoimmune.
Infectious inflammation can be triggered by viruses, bacteria, fungi, protozoa and parasites.
The most common infectious agents of meningoencephalitis:
| Bacteria | Viruses | The simplest |
| Neisseria meningitidis, Listeria monocytogenes, Rickettsia rickettsii, Rickettsia conorii, Rickettsia africae, Ehrlichia chaffeensis, Mycoplasma pneumonia, Treponema pallidum, Mycobacterium tuberculosis, Borrelia burgdorferi, Leptospira. | Epstein-Barr virus, herpes simplex virus type 1 and type 2, enterovirus, rabies virus, tick-borne encephalitis virus, West Nile virus, measles virus, chickenpox virus, mumps virus (mumps), HIV. | Naegleria fowleri, Balamuthia mandrillaris, Sappinia Diploidea, Trypanosoma brucei, Toxoplasma gondii. |
Infectious (parasitic) pathogens include Halicephalobus gingivalis from the nematode class, the causative agent of cysticercosis (Taenia solium), echinococcus.
The disease can be caused by the fungus Cryptococcus neoformans. It should be noted that meningoencephalitis of parasitic and fungal origin is extremely rare.
Autoimmune inflammation is talked about when the cause of tissue damage, in this case, the tissues of the brain and its membranes, is an attack of the own immune system. Autoimmune encephalitis can be caused by antibodies to amyloid beta-peptide proteins, anti-N-methyl-D-aspartate receptor antibodies (anti-NMDA; anti-NMDA receptor encephalitis), and some others.
Forms of the disease
The forms of meningoencephalitis are determined by its etiology: infectious, autoimmune, and also of unspecified etiology. By the nature of the course, it can be acute and subacute.
Some types of the disease have typical and atypical, that is, unusual, forms. Atypical forms are usually characterized by an even more serious prognosis, since an unusual clinical picture makes it difficult to diagnose, and therefore, to adequate treatment.
Disease stages
During meningoencephalitis, the beginning (the appearance of the first signs), the height and the outcome are distinguished. Infectious types of the disease also have a prodromal, or latent (latent) stage, which may be asymptomatic or have minor and nonspecific clinical manifestations. The latency period, that is, the time from infection to the appearance of the first signs of the disease, can last from several hours to several months, depending on the etiology. The height of the disease is characterized by severe and progressive symptoms. The outcome may be recovery or death if brain damage reaches a critical level and affects vital centers.
Some types of disease have stages characteristic of them. For example, during meningoencephalitis, three periods are distinguished: the stage of precursors (corresponding to the prodromal), the stage of arousal, and the stage of paralysis.
Symptoms
The clinical picture of meningoencephalitis is generally similar to that of meningitis. Common signs are changes in personality, behavior, thinking disturbances, and physical symptoms: intense headache, neck pain, stiff neck muscles, hypersensitivity to light and sound stimuli, and seizures. An increase in cranial pressure as a result of inflammation is manifested by visual impairment, dizziness, and nausea.
Let us consider in more detail the clinical manifestations using examples of some types of meningoencephalitis.
Tick-borne meningoencephalitis
Inflammation of the brain and its membranes, caused by a viral infection transmitted by ticks, begins acutely, with an increase in body temperature to febrile values (38 ° C and above), chills, severe malaise, headache, accompanied by nausea and vomiting, pain and aches in the muscles and joints. The initial stage is characterized by hyperemia of the face, neck and upper chest, mucous membranes, injection of the sclera (bleeding into the eyes), inhibited consciousness, which can later turn into a coma. Later, muscle weakness, paresthesia (tingling, numbness) appear, then these muscle groups undergo paresis and paralysis.

Ticks are carriers of viral pathogens of encephalitis
Herpetic meningoencephalitis
It has a prodromal (latent) period lasting several days, during which there is a growing malaise: body temperature rises, headache, nausea, sometimes vomiting, weakness, fatigue appears. Behavioral disturbances are noted, which gradually progress, as well as hypersensitivity to external stimuli, especially to smells, which can later transform into olfactory hallucinations. In some cases, the prodromal period is absent. The height of the disease is characterized by local neurological symptoms (unilateral paralysis, paresis), cognitive impairment (disorder of thinking, memory), lethargy, and the appearance of seizures.
Rabies meningoencephalitis
The onset of the disease is characterized by the appearance of anxiety, increased sensitivity to external stimuli (light, sound, tactile), a slight increase in body temperature, and sleep disturbances. Decreased appetite, dry mouth, sweating, tachycardia, sore throat when swallowing, sometimes nausea. Changes in behavior are noteworthy, the patient becomes nervous, rude, irritable, avoids contact with people.
At the stage of arousal, neurological symptoms develop, photophobia, exophthalmos, respiratory disorders appear, and body temperature rises. A symptom of hydrophobia is characteristic: the patient is thirsty, but when he tries to get drunk, he has a strong, very painful spasm of the muscles of the pharynx and larynx, this phenomenon grows, and later the spasm can be caused only by the sight of water, its murmur or mention of it. As the disease progresses, excruciating spasms of the muscles of the pharynx and larynx occur in response to any stimulus, even a breath of breeze. Patients do not have enough air, and they begin to rush, looking for a position in which relief will come, which is perceived by others as an attack of rabies. Patients may experience hallucinations, delirium. If death does not occur at this stage, the stage of paralysis develops,during which the patient becomes immobile, stops responding to light. Due to damage to the pelvic nerves, urinary and fecal incontinence develops. Body temperature continues to rise (42 ° C). And although it becomes easier for the patient to breathe and drink, this stage ends in death.
Meningococcal meningoencephalitis
The defeat of the brain and its membranes caused by meningococci is characterized by an acute onset - an increase in temperature to febrile values, intense headache, increased sensitivity to any stimuli. A characteristic feature of this disease, which distinguishes it from meningoencephalitis of another bacterial etiology, is that it is often combined with meningococcemia, i.e., the circulation of meningococci in the bloodstream. It is accompanied by the appearance of skin rashes, at first roseolous or roseolous-pustular, and later hemorrhagic, forming rather large blood-red or purple spots on the skin of an irregular shape.
Amebic meningoencephalitis
Primary amoebic encephalitis is caused by Fowler's nigleria (Naegleria fowleri), the simplest microorganism that lives in warm fresh water. Infection occurs when the amoeba, along with water, enters the nose, and then along the olfactory nerve into the brain. The latent period lasts from 2 to 6 days, after which intense headaches, attacks of dizziness, and thought disorders appear. A characteristic feature is a decrease or lack of taste and smell. Later, convulsions appear in the form of epileptic seizures, hallucinations, imbalance, ataxia (dissociation of the action of different muscle groups with preserved muscle strength). The symptomatology increases, taking on a threatening character, up to death, which usually occurs within 10 days.

The causative agent of primary amoebic encephalitis lives in warm water
Other types of amoebas cause granulomatous amoebic meningoencephalitis, which can occur subacutely, and in rare cases can become chronic with mild symptoms. More often, however, the disease begins suddenly with neurologic symptoms or skin lesions (with Balamuthia mandrillaris infection). Seizures, headache, and cognitive impairment are characteristic. Symptoms gradually increase until the onset of death, which in the case of an acute course of the disease occurs within 7-10 days, subacute - up to 120 days.
Anti-NMDA receptor meningoencephalitis
It is more common in women, sometimes associated with ovarian teratoma (which is the reason for one of the names - acute early female non-hepatic encephalitis), often observed in children and adolescents (another name for this disease is associated with acute non-hepatic encephalitis of young people). It often starts with psychiatric symptoms, which causes diagnostic errors (the disease is often mistaken for acute schizophrenia or another mental illness with similar manifestations), memory and attention impairment is noted. Later, breathing disorders, fever, convulsions, epileptic-like seizures and other neurological symptoms appear, which serves as an indication of the non-psychiatric nature of the pathology. It differs from other types of meningoencephalitis in a generally favorable prognosis.
Features of the course of meningoencephalitis in children
The course of the disease in children is similar to that in adults, perhaps the difference is in a more violent course of the disease, but also a slightly better prognosis - in children, long-term consequences are less likely to develop, and they are usually transient in nature.
The disease begins acutely, with high fever (40-41 ° C), severe headache that is not relieved by analgesics and is accompanied by nausea and vomiting that does not bring relief. The child may be inhibited or, on the contrary, agitated, small children may cry monotonously (meningeal cry). Hallucinations, stupor, coma may appear. Pronounced meningeal syndrome (stiffness of the neck muscles, the pose of a pointing dog - on the side with the head thrown back and legs pulled up to the stomach, positive Kernig and Brudzinsky symptoms, paresthesias, pain phenomena). Convulsions occur, but it should be borne in mind that seizures in children can be caused by a high fever (called febrile seizures), so they do not necessarily indicate brain damage and should only be evaluated in conjunction with other symptoms.
Diagnostics
Clinical diagnosis consists in assessing the patient's mental status, consciousness, and focal neurological symptoms. The presence of hyperthermia, seizures is determined, functional tests are carried out. When collecting anamnesis, attention is paid to recent events: past viral diseases, swimming in bodies of water with dirty water, tick or animal bites, contacts with patients, etc.
Instrumental and laboratory examination includes:
- puncture of the spinal cord with analysis of cerebrospinal fluid, i.e. cerebrospinal fluid (blood admixture, pleocytosis, and sometimes microbial agents can be detected);
- serodiagnostics (PCR, laboratory blood test to determine the type of viral pathogen);
- laboratory analysis of nasopharyngeal lavages;
- laboratory analysis of blood for the presence of specific antibodies (if an autoimmune nature of the disease is suspected);
- magnetic resonance imaging (allows you to assess the state of the brain and membranes);
- computed tomography (for the purpose of differential diagnosis);
- electroencephalogram (assessment of the degree of brain damage and its functions);
- brain biopsy.

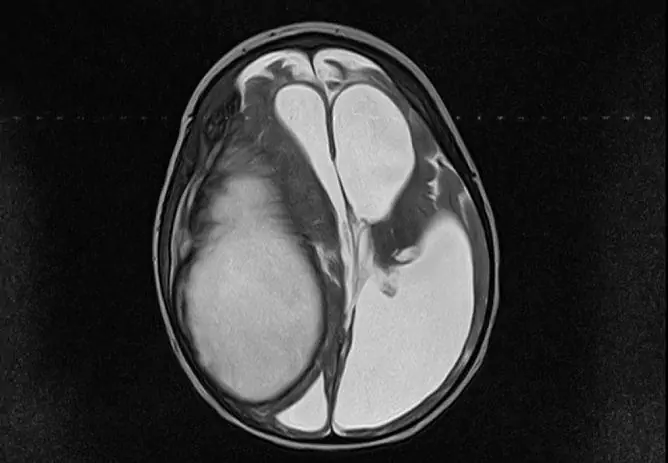
Purulent meningoencephalitis
Differential diagnosis is carried out with other diseases with similar symptoms, depending on the form. For example, amoebic meningoencephalitis can mimic a malignant tumor or abscess (purulent fusion of an area) of the brain, some types of autoimmune inflammation are similar to the manifestations of schizophrenia or drug intoxication, etc.
It is important that the disease is diagnosed accurately, with the identification of the etiological factor, since the timeliness and effectiveness of treatment depends on this.
Treatment
Suspicion of meningoencephalitis is a reason for hospitalization, treatment is carried out in a hospital setting. Measures are being taken to maintain vital functions, to prevent infectious toxic shock.
Etiotropic treatment depends on what is causing the meningoencephalitis. In case of a disease of infectious etiology, antibiotics or antiviral agents are used. Antiviral therapy should be used as early as possible.
Symptomatic treatment is prescribed, specific medications depend on the manifestations of the disease. At high temperatures, antipyretics are used, for convulsions and seizures, anticonvulsants (anticonvulsants, antiepileptic drugs) can be prescribed, with increased intracranial pressure - diuretics (diuretics).
At the recovery stage, brain stimulants, vitamin therapy, physiotherapy are prescribed.
Possible complications and consequences
The consequences of the transferred meningoencephalitis can be short-term and long-term. Both the first and the second include neurological deficits of varying severity, depending on how much the brain tissue has been damaged. These can be hearing impairments, vision, coordination, speech, gait, movement disorders, paresis, paralysis, and personality changes. To minimize the damage to the brain, quick and accurate diagnostics, timely and correct medical care, and after recovery, in most cases, neurological rehabilitation, the volume of which is determined individually, is needed.
Forecast
The prognosis is generally poor, although it varies depending on the form of the disease and the state of the patient's immune system. Poor prognostic signs include cerebral edema, status epilepticus, and thrombocytopenia. Good - normal encephalogram results.
Meningoencephalitis often leads to severe damage to brain tissue and is fatal. If the patient can be saved, often he is left with a lifelong neurological deficit, the consequence of which is disability.
Prevention
The specific and most effective preventive measure is vaccination against certain forms of meningoencephalitis. There are vaccines against meningococcus, the causative agent of tuberculosis, influenza virus, measles, tick-borne encephalitis and a number of others.
The non-specific methods of prevention include maintaining the body's defenses at a high level, which includes following the rules of a healthy lifestyle, as well as observing the rules of sanitation and personal hygiene.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!