- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Intervertebral hernia
The content of the article:
-
What is pathology
- Features of the structure of the spine
- The mechanism of development of the disease
- Why pathology develops
- Kinds
-
Symptoms of the intervertebral hernia
- Cervical
- Chest
- Lumbosacral region
- Consequences and possible complications
- Diagnostic methods
-
How to get rid of the disease
- Treatment without surgery
- Indications for surgical treatment
- Types of surgery
- Postoperative period
- Video
Herniated discs are one of the most common causes of back pain. Pathology is characterized by a protrusion of the intervertebral disc located between the vertebral bodies. In most cases, a hernia is a complication of osteochondrosis. When symptoms appear, you need to consult a doctor and undergo an examination, early detection of pathology increases the effectiveness of treatment. For treatment, conservative methods are used, if there is no effect, an operation is performed.
What is pathology
Herniated disc is a disease in which the nucleus pulposus of the intervertebral disc bulges out. The mechanism of development of the disease is associated with the structure of the spine.

Herniated disc is formed due to degenerative processes in the disc that separates the vertebrae
Features of the structure of the spine
The vertebral column consists of 33-34 vertebrae, which are interconnected by elastic discs. Thanks to the latter, the mobility and flexibility of the spine is ensured.
The disk structure is as follows:
- nucleus pulposus - located inside, soft, has a gel-like consistency and is 90% water;
- annulus fibrosus - located outside, solid and durable, it surrounds and delimits the nucleus pulposus.
The discs of the cervical spine are smaller, the lumbar discs are the largest.
The mechanism of development of the disease
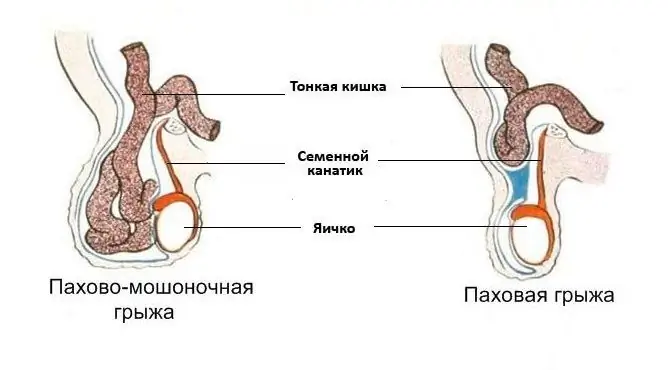
Normally, each intervertebral disc is located strictly between the bodies of two vertebrae. If it goes beyond this interdisk space, a spinal hernia develops.
The development of the disease is usually associated with disc degeneration (wear). The annulus fibrosus loses its elasticity, tears and cracks may develop. All this leads to protrusion of the nucleus pulposus.
Why pathology develops
There is no single reason that would lead to the development of the disease. In most cases, the formation of a hernia is associated with osteochondrosis of the spine. This is a degenerative-dystrophic disease in which the intervertebral disc loses its elasticity and dries out. Its height decreases, so any physical activity can lead to injury.
What factors increase the likelihood of displacement of the intervertebral disc:
- lifting weights;
- sharp twisting movements;
- prolonged sitting position;
- obesity;
- excessive physical activity;
- overloads of the spinal column associated with flat feet and wearing uncomfortable shoes;
- abrupt cessation of regular exercise.
Genetic predisposition also plays a role. A hernia of the intervertebral space can develop not only as a complication of osteochondrosis, but also with trauma and curvature of the spine, in persons with developmental anomalies leading to overload of the spinal column.
Kinds
Any part of the spine can be affected, but most often the lumbosacral and cervical. Clinical symptoms depend on localization, each type of disease has its own symptoms. There are the following types of pathology, taking into account the location:
- Lumbosacral hernia is the most common. In 90% of cases, the protrusion is localized at the L4-L5 and L5-S1 levels.
- The cervical spine is the second most common.
- The thoracic region is extremely rare.
Depending on the stage of hernia formation, the following types are distinguished:
- prolapse;
- protrusion;
- extrusion;
- disk sequestration.

A hernia is a protrusion of the nucleus pulposus of the disc beyond the annulus fibrosus
Symptoms of the intervertebral hernia
At the beginning of the formation of a hernia, the disease usually does not manifest itself in any way, the person does not suspect that he is sick. Symptoms appear when the bulge compresses the surrounding nerves and blood vessels. Clinical manifestations depend primarily on the type of disease.
Cervical
The main symptom of the disease is pain in the back of the neck. Pain sensations increase with exertion, decrease in a supine position. The pain is dull in nature, it can radiate to the upper limb.
In addition to pain syndrome, when nerves are compressed, a violation of innervation occurs:
- numbness of the fingers;
- trophic skin changes;
- periodic dizziness;
- headache;
- fluctuations in blood pressure.
The severity of symptoms depends on the size of the bulge and the degree of nerve compression.
Chest
The pain is most often localized in the upper back. It increases with physical exertion, prolonged stay in an uncomfortable position. The pain can also be localized in the chest region, resembling heart or stomach diseases.
Lumbosacral region
The pain is localized in the lower back, often radiating to the lower extremities, sacrum, genitals. Painful sensations increase with exertion, pass at rest.
There are other symptoms associated with impaired innervation:
- numbness and tingling in the leg;
- muscle weakness in the lower limb;
- decreased sensitivity;
- pelvic disorders - urinary and fecal incontinence, erectile dysfunction.
The localization of symptoms can be different - only the thigh, thigh and lower leg, from the buttocks to the fingertips. It depends on which nerve is pinched.

The main symptom with which patients suffering from an intervertebral hernia turn to a doctor is pain in the spine
Consequences and possible complications
With early detection of the disease and the beginning of treatment, the prognosis is favorable. In about 75% of cases, the condition improves within 4-6 weeks, but there is a high risk of relapse.
The clinical picture is not limited to only the main symptoms. In some cases, complications develop that change the symptoms. Complications can be different, depending on which part of the spine the hernia is located in.
| Localization | Typical complications |
| Cervical |
The most common complication is vertebral artery syndrome. The vertebral artery is compressed, which supplies the brain. Clinically, this is manifested by the following symptoms: · noise in ears; · dizziness; · loss of consciousness; • flashes of light in the eyes; • lack of coordination. In severe cases, vertebral artery syndrome can cause transient ischemic attacks (TIAs), a transient violation of the blood supply to the brain. |
| Chest | A hernia in the thoracic spine can compress the visceral branches that innervate the internal organs. Therefore, a complication of the disease can be a disruption of the esophagus, bronchi, liver, pancreas, and intestines. |
| Lumbosacral region | Most often it is complicated by radicular syndrome (radiculopathy). This is a condition in which the spinal root is compressed, which leads to severe pain syndrome. |
Another complication that can develop in all types of the disease is discogenic myelopathy. This is a condition in which a bulging disc causes the spinal canal to narrow and compress the spinal cord. There are motor or sensory disorders on the one hand:
- paresis of the lower limb (right or left) with loss of tendon reflexes;
- loss of sensitivity;
- dysfunction of the pelvic organs - urinary and fecal incontinence.
Over time, the condition worsens, the changes become irreversible.
Diagnostic methods
It is possible to suspect the presence of a spinal hernia by the characteristic symptoms, but additional examination is required to make a diagnosis. Magnetic resonance imaging (MRI) is considered the gold standard, but sometimes other tests are required.
| Diagnostic method | Who is shown | Explanation |
| Plain radiography | All sick | An accessible, but insufficiently informative research method. On the plain X-ray, you can see signs of osteochondrosis and anomalies in the development of the spine, but it will not be possible to diagnose the pathology of the intervertebral discs. |
| Magnetic resonance imaging (MRI) | All sick | MRI or CT will help to detect pathology. Soft structures such as an intervertebral disc are better visualized on MRI. The study will help determine the location and size of the protrusion. |
| Doppler ultrasound (USDG) of vessels | With damage to the cervical spine | The protrusion of the disc in the cervical spine can squeeze not only the nervous tissue, but also the vessels. This is an indication for conducting vascular studies (USDG of vessels). |
| Electrocardiography (ECG) | With damage to the thoracic spine | When a disc is involved in the thoracic region, symptoms may mimic angina pectoris. To exclude cardiological pathology, an ECG is performed. |

MRI is the main method for diagnosing intervertebral hernias
How to get rid of the disease
There are several treatments for the disease. Conservative therapy or surgery can be used. The choice of therapeutic tactics depends on several factors - the size and location of the protrusion, the severity of symptoms, the presence of complications, and the duration of the disease.
Treatment without surgery
In 90% of cases, the disease can be successfully treated with conservative treatment. Conservative therapy is of a complex nature - medications, paravertebral blockades, physiotherapy procedures and physiotherapy exercises are prescribed. The duration of the course of treatment should be at least 1 month.
| Treatment method | Explanation | |
| Drug therapy | Non-steroidal anti-inflammatory drugs (NSAIDs) |
NSAIDs are prescribed to relieve pain and relieve inflammation. Systemic NSAIDs are used: Meloxicam; Diclofenac (Dicloberl); Ibuprofen · Naproxen. |
| Muscle relaxants |
Central muscle relaxants are prescribed to relieve muscle tension, since muscle hypertonicity aggravates nerve entrapment. The following drugs are used: · Mydocalm; · Miaxil; · Toccata. |
|
| B vitamins | B vitamins are prescribed to improve the trophism of nerve fibers. | |
| Paravertebral blockade | Paravertebral blockade is prescribed to relieve pain. The essence of the procedure is the introduction of anesthetics and glucocorticoids into the paravertebral tissues. | |
| Physiotherapy |
In the acute period of the disease, the following physiotherapeutic methods are used: · UHF; · Ultraphonophoresis with hydrocortisone; · Electrophoresis. They are aimed at reducing inflammation and swelling, and improving blood circulation. After relief of acute manifestations, reflexology and mud therapy are used. Traction therapy has a good effect, which is aimed at increasing the intervertebral distance and reducing the load on the intervertebral disc. |
|
| Physiotherapy | An important component of treatment is physiotherapy exercises (exercise therapy). With the help of special exercises, you can achieve stretching of the spine, strengthening the muscular frame. Thus, the load on the affected disc is reduced. In addition to exercise therapy, massage is used to improve blood circulation and reduce muscle tension. | |
The effectiveness of treatment is also influenced by the observance of general recommendations:
- sleeping on a hard surface or floor;
- choose an orthopedic pillow;
- exclude heavy physical activity;
- move more during the day.
Indications for surgical treatment
Surgery is the most effective and radical method of treatment, but surgical intervention is inevitably associated with a high risk of postoperative complications, so this treatment is not indicated for everyone. Surgery is required in about 10% of cases.
In what cases is surgical intervention indicated:
- Pain syndrome does not stop within 1.5 months of conservative treatment.
- The disease was complicated by discogenic myelopathy, vertebral artery syndrome.
- Dysfunction of the pelvic organs (urinary and fecal incontinence, erectile dysfunction) is present.
The decision on the need for the operation is made on an individual basis. The patient's age, general condition, and the presence of concomitant diseases are also taken into account.

10% of patients with intervertebral hernia require surgery
Types of surgery
The purpose of surgery may be to remove a hernia or decompress the spinal cord (if complications develop). Treatment can be done with laminectomy, microdiscectomy, or endoscopic hernia removal.
| Operation name | Advantages and disadvantages | Explanation |
| Laminectomy |
The only advantage is that there is no need for special equipment. Disadvantages: · Trauma; · High risk of postoperative complications; · Long recovery. |
Laminectomy is the most traumatic treatment. During the operation, the vertebral arch is removed. Its removal leads to the expansion of the cavity of the spinal canal and eliminates its compression. Currently, laminectomy is rarely used because less invasive treatments are available. |
| Microdiscectomy | The advantages include the ability to remove a hernia of any size and location. Disadvantages: relative trauma, risk of complications (but less than with laminectomy). | Microsurgical hernia removal (microdiscectomy) is increasingly used. The operation is performed under general anesthesia, a 3-4 cm incision is made on the skin. Hernia removal is performed using a microscope. |
| Endoscopic removal | The main advantage is low invasiveness. The disadvantage is that it is impossible to remove large hernias. | The least invasive method of treatment is endoscopic hernia removal. The operation is performed under anesthesia using a special device - an endoscope. The device is inserted through small incisions in the skin. |
Postoperative period
Recovery time depends on the type of surgery (from 2-3 days for endoscopic surgery to several months for laminectomy). It is recommended to wear a semi-rigid corset for 1-2 months after the operation. Physical activity is limited to 1 month.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.